by Thomas Lethenborg | Nov 15, 2016 | News, Press releases
Copenhagen, Denmark – 15 November 2016. Monsenso announced today that the Norwegian hospital, Lovisenberg Diakonale Sykehus, will begin a pilot study with the Monsenso mHealth solution that aims to reduce hospital readmissions of individuals with bipolar disorder. Lovisenberg was signed up as a customer by Computas, Monsenso’s partner in Norway.
The pilot study, which will include individuals with bipolar disorder, aims to reduce hospital readmissions by using the Monsenso mHealth solution to intervene at an early stage.
Thomas Lethenborg, CEO at Monsenso, said that Lovisenberg would conduct a ten-month pilot study to determine if the solution should be widely implemented with other mental illnesses.
“Lovisenberg is committed to finding innovative solutions that help them provide better care to their patients in a more cost-efficient way. With the implementation of the Monsenso mHealth solution, a patient’s historical, aggregated data will be available more easily,” Mr Lethenborg added.
Kim Petersen, Executive Director at Computas AS, said “We are thrilled to have signed up our first customer with Monsenso. This type of technology gives new opportunities for the integration of mobile health into the existing mental health services in Norway; and I am confident that once clinicians start experiencing the clinical and financial benefits of implementing the solution, we will sign up more customers in no time!”
Andreas Joner, Head of Clinic at Lovisenberg, said the trial would allow them to investigate how a remote patient monitoring solution can be used to improve patient care and patient engagement.
“The Monsenso mHealth solution will help us to access and analyse data in a more efficient way. Besides, since most people carry their smartphones all the time, patients can answer their self-assessments and clinical questionnaires wherever they are, without feeling self-conscious,” said Andreas Joner.
The Monsenso mHealth solution for mental illnesses is based on a triple-loop treatment model that connects patients, carers and clinicians and has the potential to reduce hospital readmissions of bipolar patients.
Patients use a smartphone to fill in routine self-assessments that reveal their current state of mind and collect sensor data. The smartphone app also works as a self-help tool that allows patients to manage their symptoms and the behaviours that trigger those symptoms. Carers are also given a smartphone that allows them to assess the overall well-being of the one they care for, and make notes that are shared with the patient and the clinician.
Clinicians use a web portal that provides historical information on each patient, including routine self-assessments and clinical questionnaires. The portal also allows them to obtain an overview of their patients’ illness progression, symptoms, medication compliance, and medical record keeping.
With more than 1300 employees, Lovisenberg Diakonale Sykehus delivers effective treatment and outpatient care across its multiple sites. The hospital provides specialist care in mental health.
For additional information contact:
Jennifer Highland
Marketing and Communications Manager
Monsenso
+45 81 71 7713
highland@monsenso.com
Tone Hærem
Communications Director
Lovisenberg Diakonale Sykehus
tone.harem@lds.no
Pål Vermund Knudsen
Sales Director
Computas AS
pal.vermund.knudsen@computas.com
About Lovisenberg Diakonale Sykehus
Lovisenberg Diaconal Hospital provides specialised health care services in mental health and internal medicine for 180,000 inhabitants of four City Districts in Oslo (inner city). In addition, mental health services are offered to several other city boroughs. The surgical department performs scheduled operations, and has one of the leading orthopaedic units in Norway. The hospital has 234 beds, more than 2,000 employees, and an extensive out-patient facility. It is a non-profit, privately owned organisation, all services provided are within Public Health. Our mission is to offer diagnostics, treatment, and follow up services of a high quality to all our patients, with equality and respect. Being innovative and finding new solutions is part of this.
About Computas
Computas is an international IT solutions provider based in Norway, delivering solutions all over the world. We deliver services and solutions for work processes and collaboration. Our core competence is systems development, architecture and integration, project management and consulting. We have unique experience, deliver high quality in all projects, and work closely with customers to make the best solutions. The health care system in Norway is changing, and there is a need for smart solutions that can ensure quality and improve the efficiency of health services. The key to solving these challenges is through better use of IT. We are prepared to contribute with our expertise and our solutions aimed at patients and health care workers. We have delivered everything from work process solutions to apps to help the health sector to work more efficiently and to help patients to have better safety.[/vc_column_text][vc_column_text]You can download this article as PDF in English, Danish and Norwegian

by Thomas Lethenborg | Aug 30, 2016 | News, Press releases
Copenhagen, Denmark – 30 August 2016. Monsenso, the Copenhagen-based technology company developing mHealth solutions for mental illnesses, today announced a partnership with The Black Dog Institute in Australia.
Black Dog Institute is a pioneer in the identification, prevention and treatment of mental illness and the promotion of well-being. The Institute will conduct feasibility studies to determine if the Monsenso mHealth solution can be used to collect much needed data for a number of large-scale mental health trials.
“The mission of Monsenso and that of Black Dog are highly aligned. We both aim to enable better mental health care through innovation and science, therefore this is an exciting moment for both parties” said Thomas Lethenborg, CEO at Monsenso. “Monsenso is looking to build sustainable, long-term partnerships, with the ultimate goal of delivering better care, to more people, and at lower cost.”
As part of the on-going collaboration between Monsenso and the Black Dog Institute, Mads Frost, Chief Product Officer of Monsenso, has been invited to participate as a guest-speaker at the conference “Humans and Machines: A Quest for Better Mental Health” organised by Black Dog.
Helen Christensen, Director of the Black Dog Institute, said the trial would allow them to collect real-time information using a device that most people carry at all times – their Smartphone. “Our focus will be on collecting self-reported daily mood ratings and activity data that may be used to predict changes in mental health conditions over time. Ultimately these sorts of tools can be used to deliver real time assistance to those in distress at the time they most need help. However, like all good research and development projects, our aim is to test the validity of these approaches; their feasibility and the extent that they can provide better health care services. Ultimately, we hope to use these sorts of tools in our national programmes involving youth mental health and suicide prevention.”
The Monsenso mHealth solution for mental illnesses holds a CE mark and a TGA certification and it has been technically and clinically validated in clinical evaluation studies and randomised clinical trials. Furthermore, Monsenso is in the process of obtaining the ISO 13485 and ISO 27001.
For additional information contact:
Jennifer Highland
Marketing and Communications Manager
Monsenso
+45 81 71 7713
highland@monsenso.com
Gayle McNaught
Head of Public Affairs
The Black Dog Institute
g.mcnaught@blackdog.org.au
About The Black Dog Institute
The Black Dog Institute is a not-for-profit organisation which is internationally recognised as a pioneer in the identification, prevention and treatment of mental illnesses, and the promotion of well-being. We are dedicated to improving the lives of people affected by mental illness through the rapid translation of high quality research into improved clinical treatments, increased accessibility to mental health services and delivery of long-term public health solutions. Our unique approach incorporates clinical services with our cutting-edge research, our health professional training and community education programs. We combine expertise in clinical management with innovative research to develop new, and more effective, strategies for people living with mental disorders. For more information visit www.blackdoginstitute.org.au
You can download this article as PDF in English and Danish

by Thomas Lethenborg | Jun 21, 2016 | Blog, Mental Illness, mHealth
According to a recent statement by the new American Heart Association (AHA), major depressive disorder and bipolar disorder should be recognized as moderate risk factors for atherosclerosis and early cardiovascular disease. [1]
In 2011, the National Heart, Lung and Blood Institute identified four conditions (chronic inflammatory disease, human immunodeficiency virus, Kawasaki disease, and nephritic syndrome) that lead youths to a mild risk of developing cardiovascular disease before they reach 30. [2]
The statement released a few days ago, reveals that depression and bipolar disorder meet the same criteria as these conditions. Moreover, these two behavioural disorders are more widespread than the previous mentioned conditions combined.
These studies showed evidence of a link between paediatric depression and bipolar disorder with premature cardiovascular mortality. Cardiovascular risk factors for these teens include obesity, insulin resistance and diabetes, dyslipidemia, and hypertension.[1] According to the statement, depression and bipolar disorder are the first- and fourth-most disabling conditions, among adolescents worldwide.
After the report had been unveiled, researchers from schools around the U.S. and Canada looked at existing studies on mood disorders in people under the age of 30. Researchers looked specifically into youths suffering from depression or bipolar disorder with cardiovascular markers such as high pressure and cholesterol. They found a significant connection between having depression or bipolar disorder and increased odds of high blood pressure, high cholesterol, obesity (especially belly fat), type 2 diabetes, and hardening of the arteries. [3]
This discovery denotes that healthcare providers should track physical activity levels and food intake as well as metabolic monitoring is crucial for these young patients as a preventive measure.
However, to monitor cardiovascular markers, physical activity and food intake, of thousands of young patients who also suffer from mental illness is not an easy task. Although, there are hundreds of smartphone applications tracking physical activity and counting calories, these apps are personal, and clinicians do not have access to an individual’s data. Nevertheless, with the Monsenso mobile health (mHealth) solution, this cumbersome task becomes easy and achievable.
The Monsenso mHealth solution enables clinicians to access a patient’s data on a daily basis. Every day, youths would be reminded to fill in a self-assessment with important information that could include the number of hours they slept, the amount of unhealthy food they have eaten, and if they realized any physical activity throughout their day. Additionally, the smartphone can also collect physical activity and mobility data, based on the smartphone’s inbuilt accelerometer and GPS locator.
The Monsenso mHealth solution, especially designed to monitor behavioural data of patients suffering from mental illness, can in this way help clinicians monitor any unhealthy habits of patients with risk of developing cardiovascular disease.
Further, with the customisable action plans, each youth could follow “contingency plans” if they experience some symptoms related to their mental illness or if they have engaged in unhealthy activities. For example, a special trigger could set up if a youth has indulged in unhealthy food for several days in a row, or has had a low level of physical activity. The action plan listed for this trigger could then encourage individuals to engage in physical activities and and to try to avoid sugar and fat during the upcoming week.
References:
[1] Browser,D Medscape. Depression, Bipolar Disorder in Teens are CVD Risk Factors: AHA (2015, August 10) http://www.medscape.com/viewarticle/849312
[2] American Heart Association. Young people with mood disorders have increased risk of developing early cardiovascular disease (2015, August 11)
http://blog.heart.org/young-people-with-mood-disorders-have-increased-risk-of-developing-early-cardiovascular-disease/
[3] Walton, A Forbes. Teens with depression, bipolar disorder, should be screened for heart disease, experts say. (2015, August 11) http://www.forbes.com/sites/alicegwalton/2015/08/11/depressed-teens-may-be-at-higher-risk-for-heart-disease/
Goldstein BI, Carnethon MR, Matthews KA, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease. Circulation 2015.

by Thomas Lethenborg | May 24, 2016 | mHealth
In 2011, the European Union commissioned the Impact Consortium to write a report in regards to “The long-term mental health care for people with severe mental disorders.”
This blog post explores the principal issues involved in the long-term care of individuals suffering from severe mental systems mentioned in the report, and how some of these issues can be partially solved with the use of mobile health technology.
The long-term care of people suffering from severe mental disorders is one of the most significant challenges for the health care systems since the impact they have on individuals, families and societies is huge.
According to the report, schizophrenia has an estimated point prevalence of 0.4% and a lifetime risk of 1%, which means that 1 in every 100 people will suffer from schizophrenia during their lifetime. It is the 7th most important illness in terms of years lived with disability, accounting for 2.8% of disability caused by all illnesses. For people aged 15 to 44 years, it is the 3rd most important disease, accounting for 4.9% of disability resulting from all illnesses.
During the last few decades, the European Union has made a huge effort to overcome these barriers and to ensure high-quality longer-term care for people with severe mental disorders. These efforts started in the 60’s with the development of new pharmacological treatments for psychoses, which radically changed the prognosis of severe mental illness. In the 70’s and the 80’s, there was an emergence of new psychosocial interventions and new concepts of mental health care organisations [1].
Nowadays, there is a need to shift the health care model. The transition from traditional large psychiatric institutions to modern comprehensive community-based models of care, including acute patient units at general hospitals [1].
According to the report, this shift is necessary due to the following reasons:
- Accessibility to mental health care of people with longer-term mental disorders is much better with community-based services than with the traditional psychiatric hospitals
- Community-based services are associated with greater user satisfaction and increased met needs. They also promote better continuity of care making possible to identify and treat more often early relapses
- The community-based services protect the human rights of people with mental disorders and prevent stigmatisation of those people
- Studies comparing community-based services with other models of care consistently show significantly better outcomes on adherence to treatment [1]
However, European healthcare systems need to make lots of alterations if they want to provide accessible, effective, high-quality and long-term care to people suffering from severe mental disorders.
Challenges of the transition to new comprehensive community-based models of care
One of the main reasons why the development of long-term mental health services is insufficient is due to the lack of coordination between the different health services. A close coordination, and even joint funding and management of health and social care services is fundamental to cope with the new challenges European mental health systems are now facing. [1].
According to the report, these are the key principles to organise mental health services:
- Accessibility: Essential mental health care should be available locally, including outpatient and inpatient care, as well as rehabilitative care. Local services provide continuity of care in a satisfactory manner.
- Comprehensiveness: Mental health services should include all facilities and programmes required to meet the essential care needs of the populations.
- Coordination and continuity of care: People suffering from severe mental disorders often find it extremely difficult to gain access to various basic services; therefore, it is crucial that services work in a coordinated manner. This coordination should also include services that are not directly related to health, such as social services and housing services.
- Effectiveness: Service development should be guided by evidence of the effectiveness of particular interventions. For example, there is a growing evidence base of effective interventions for many mental disorders, among them depression, schizophrenia and alcohol dependence.
- Equity: A person’s access to services of good quality should be based on need. It is quite often that the people who need these type of services the most are the least able to ask for help.
- Respect for human rights: Services should respect the autonomy of persons with mental disorders, and encourage such persons to make decisions affecting their lives and treatment [1].
The solution
The Monsenso mobile health solution can facilitate five of the six points mentioned in the report to organise mental health services in an optimal way.
- Accessibility: With mobile technology and telehealth, care providers can reach patients living in remote locations at a minimal cost. These technologies offer care providers more flexibility to deliver health care while on-the-go or from different locations—expanding the clinic’s service offerings [2].
- Coordination and continuity of care: The Monsenso mobile health solution can facilitate and support the care of patients suffering from severe mental illnesses from community-based models. Due to its cloud-based model and unlimited scalability, patient records can be accessed by multiple organisations such as psychiatric institutions, general practitioners, and social services, among others.
- Effectiveness and equity: With help of the Monsenso smartphone app, care providers can identify on a daily basis triggers and early warning signs of all patients in the system. With the Monsenso mHealth solution clinicians can prioritize caring for individuals who need immediate attention and continue to monitor individuals who are stable. According to the National Institute of mental health, early intervention is critical to treating mental illness before it can cause tragic results such as serious impairment, unemployment, homelessness, poverty, and suicide [4].
- Respect for human rights: The Monsenso smartphone app enables patients to fill in daily self-assessments and write notes about how they feel. The information collected from these assessments is shared with the clinic, allowing individuals to be more involved with their treatment. The Monsenso smartphone app also provides individuals with customised action plans that act as guidelines in case their symptoms appear enabling individuals to take responsibility for their behaviours and actions.
References:
[1] The long-term mental health care for people with severe mental disorders. J.M Caldas de Almeida, H. Killaspy. Prepared under service contract with the Impact Consortium by the European Commission. 2011.
http://ec.europa.eu/health/mental_health/docs/healthcare_mental_disorders_en.pdf
[2] Increasing access to behavioural health care through technology. The U.S. Department of Health and Human Services Health Resources and Services Administration (2013, February).
http://www.hrsa.gov/publichealth/guidelines/behavioralhealth/behavioralhealthcareaccess.pdf
[3] Directors Blog: SAMHSA and NIMH partner to support early intervention for serious mental illness. P. Hyde and T. Insel. National Institute of Mental Health Blog (2014, June 17)
http://www.nimh.nih.gov/about/director/2014/samhsa-and-nimh-partner-to-support-early-intervention-for-serious-mental-illness.shtml
[4] Evidence based treatment for first episode of psychosis: Components of coordinated specialty care. PHD R. K. Heinssen. RAISE NIMH (2014, April 14).
http://www.nimh.nih.gov/health/topics/schizophrenia/raise/nimh-white-paper-csc-for-fep_147096.pdf
by Thomas Lethenborg | Oct 15, 2015 | mHealth
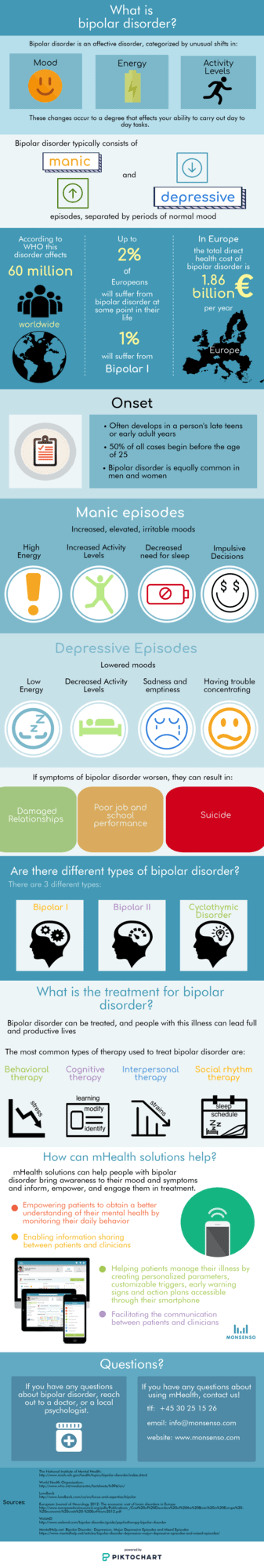
What is bipolar disorder?
Bipolar disorder is an affective disorder that is categorized by unusual shifts in mood, energy, and activity levels.
We have made an infographic, so you can get a better insight into what bipolar disorder is.
by Pauline Hansen | 17. October 2023 | Blog, Shape Up | 0 Comments
Monsenso has moved on from scrum and are now using the shape up method. This has meant changes …. In a good way.
by Thomas Lethenborg | 26. April 2023 | Blog, mHealth | 0 Comments
Over the past decade, public spending on health in Denmark has been above the EU average. But how does Denmark decide which new treatment approaches to spend money on, and does the societal impact of healthcare measures play an equally important role as their economic impact?
by Thomas Lethenborg | 21. April 2023 | Blog, Mental Illness | 0 Comments
April is Stress Awareness Month, which aims to shine light on stress and its consequences on our well-being, removing stigma and shame around mental health.
by Thomas Lethenborg | 30. March 2023 | Blog, Mental Illness | 0 Comments
March 30th is World Bipolar Day. The awareness day aims to inform about the mental illness and the struggles it can cause for individuals suffering from it, improving sensitivity and eliminating social stigma.
by Thomas Lethenborg | 9. March 2023 | Blog, mHealth, Patient Engagement | 0 Comments
The input from both end-users and clinicians is a crucial part of the design phase in the PhaseV project, where Monsenso and partners will develop a range of new digital health solutions for future clinical trials.
by Thomas Lethenborg | 28. February 2023 | mHealth, News | 0 Comments
How do patients who have received psychiatric treatment for depression experience the sector transition into the primary sector? And what are their needs for treatment and care from different healthcare sectors? The DEPRIC research project is now trying to find answers and thereby develop a new treatment model for depression across healthcare sectors in Denmark.
by Thomas Lethenborg | 15. December 2022 | mHealth, News | 0 Comments
Together with a European consortium of partners, Monsenso has received a grant letter on a new community-based intervention project that includes development and trial of a digital health intervention delivered on Monsenso’s platform to prevent mental illness among vulnerable groups.
by Thomas Lethenborg | 13. December 2022 | mHealth, News | 0 Comments
Monsenso and a consortium of partners have received a grant letter from a funding entity to develop and trial a new, AI-enabled personalised therapy concept for people with mental disorders.
by Thomas Lethenborg | 12. December 2022 | Blog, Mental Illness | 0 Comments
In order to fight non-communicable diseases and support the people suffering from them, the European Commission has launched the Healthier together – EU Non-Communicable Diseases Initiative (EU NCD Initiative), aimed at covering the period from 2022 to 2027.
by Thomas Lethenborg | 1. December 2022 | mHealth, News | 0 Comments
Monsenso’s new product enhancements entail an improved and even more intuitive user interface of the solution’s patient app and clinical web portal.