Monsenso signs contract with private Danish psychiatric clinic Appia Klinikken in Søborg
Monsenso signs a contract with the private Danish psychiatric clinic Appia Klinikken in Søborg, Zealand. The Monsenso digital health solution will be implemented at the beginning of 2023 and will be used to support patients and clinicians at the clinic.
Appia Klinikken is a Danish specialist psychiatric clinic offering treatment and support to individuals suffering from mental illness. Though the clinic has a focus on child and adolescent mental health, it offers treatment to individuals of all age groups.
The team of psychologists and psychiatrists at Appia Klinikken is led by specialist psychiatrist Mie Bonde, who “is professionally recognized for her holistic approach and for her work with clients with ADHD and/or ASD diagnoses, as well as clients with abuse combined with diagnosis(es)” [1].
The Monsenso solution will be used at Appia Klinikken for two different purposes. Primarily, the Monsenso solution will be used to screen patients while they are waiting for treatment and to monitor them during treatment. Secondly, the Monsenso solution will be used to collect data for effect documentation of a newly established type of treatment called “hypnotherapy” and for use of medication.
Specialist psychiatrist Mie Bonde says: “The Monsenso digital health solution will not only enable us to support patients more actively during treatment, but also to give patients information on how to reduce stress while they are still waiting to receive treatment. Waiting lists are something we cannot avoid entirely, but tools like the Monsenso solution enable us to make them more proactive”.
——————————————————————————————————————————-
About Monsenso
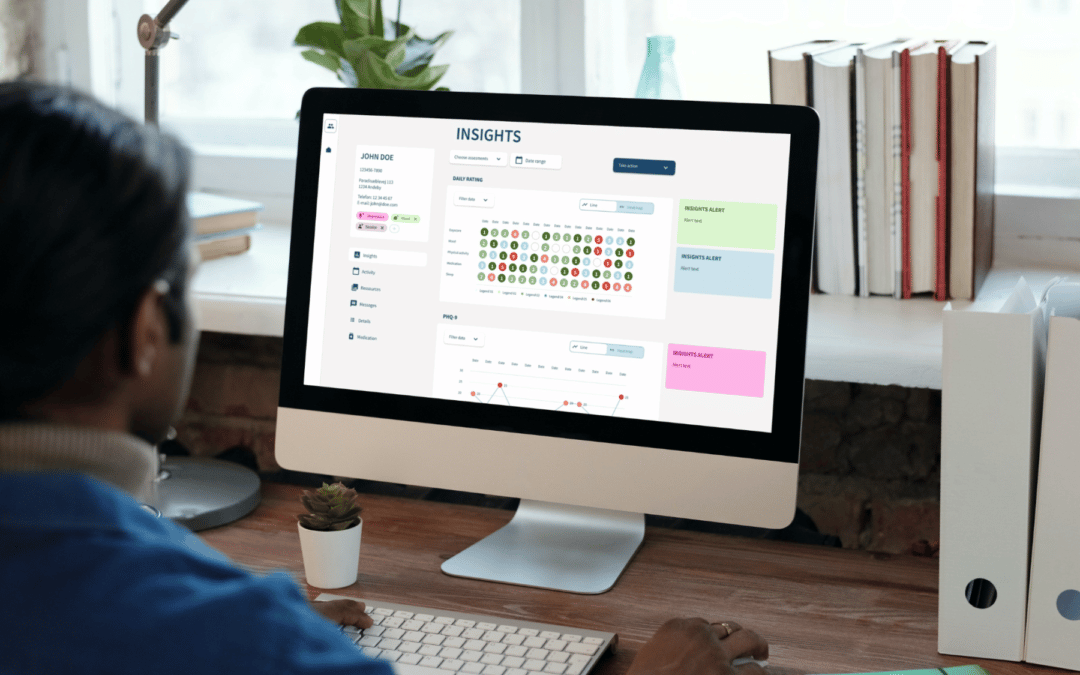
Monsenso is an innovative technology company offering a digital health solution used for decentralised trials, remote patient monitoring and treatment support. Our mission is to contribute to improved health for more people at lower costs by supporting treatment digitally and leveraging patient-reported outcomes data. Our solution helps optimise the treatment and gives a detailed overview of an individual’s health through the collection of outcome, adherence, and behavioural data. It connects individuals, carers, and health care providers to enable personalised treatment, remote care, and early intervention. We collaborate with health and social care, pharmaceuticals, and leading researcher worldwide in our endeavours to deliver solutions that fit into the life of patients and health care professionals. To learn more visit www.monsenso.com.
References:
[1] Appia Klinikken (n.d.). Appia Klinikken – Vejenes dronning.
https://www.appia-klinikken.dk/