The Momentum Trial: How digital tools can support patient-centered care & shared decision-making
In the delivery of mental health services, shared decision-making (SDM) is increasingly becoming more important [1]. SDM can be defined as a collaborative process between patient and health care provider, enabling joint treatment decisions and patient-centered care [2]. Research suggests that in mental healthcare, SDM could “contribute to recovery-oriented care by inviting the patient to have more control and be more involved in their treatment decisions” [2].
However, many mental health care providers are still reluctant to incorporate SDM into their treatment offers, as they believe it to be unfit for individuals suffering from severe mental illness, as well as to be time-consuming and thus a burden [3,4]. To overcome these challenges of incorporating SDM into daily practices, healthcare professionals have been encouraged to utilize “tools to support the SDM process” [2].
Increased focus has thus been placed on how digital interventions could support SDM in mental healthcare [2]. The Momentum Trial is a study investigating how using a smartphone app as a support tool could help “individuals suffering from schizophrenia-spectrum disorders in an outpatient treatment setting” [5].
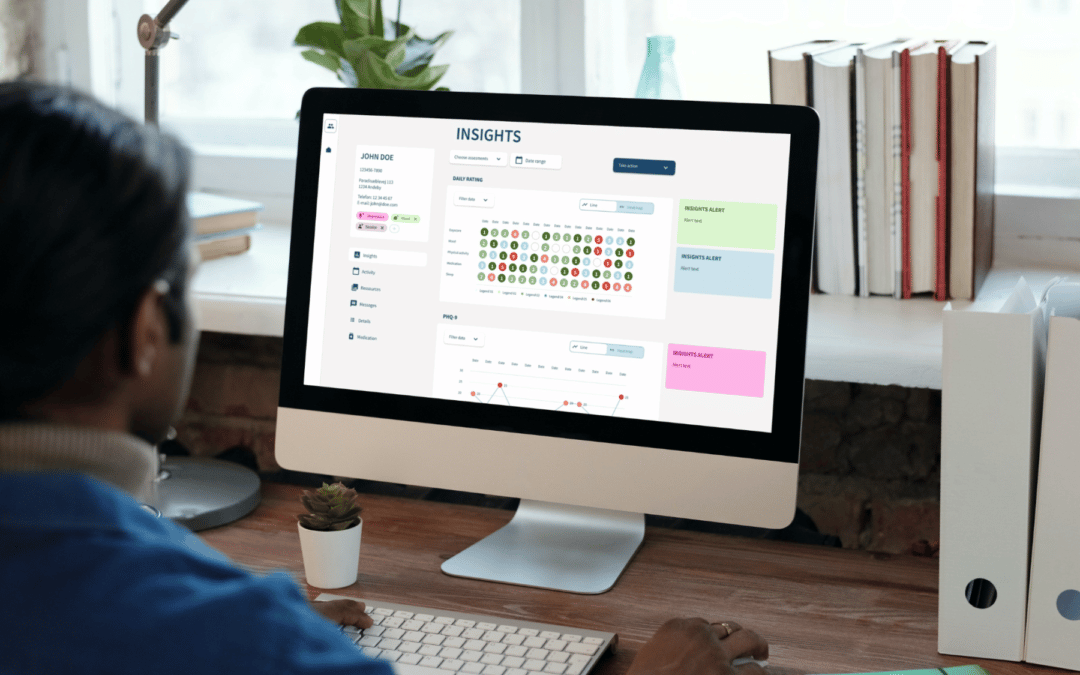
During the trial, 194 participants were randomized either to receive “specialized early intervention treatment with the Momentum app” (intervention group) or to receive regular treatment without a smartphone app (control group) [5]. The Monsenso digital health solution, consisting of a patient app and a clinical web portal, was used for the intervention group. The Monsenso solution provided tools such as psychoeducational material, daily self-assessments, and action plans in the patient app, as well as patient insights in the clinical web portal [2].
As a primary outcome, it was investigated whether the individuals from the two groups would show a difference in self-perceived patient activation. Patient activation can play an important role in successful SDM processes, as patients who are more active and engaged in their treatment “feel confident when collaborating with their provider, and have the knowledge and skills to manage their condition” [2].
As secondary outcomes, it was investigated whether the individuals from the two different groups would show a difference in the self-perceived feeling of hope and optimism, self-efficacy, confidence in communicating with their provider, therapeutic alliance between the patient and provider, feeling prepared to make a treatment decision, and satisfaction with treatment [2].
Results were evaluated at baseline, as well as 3 and 6 months post-baseline. Promisingly, the Momentum Trial showed a significant effect of a digital SDM tool on the subjective level of patient activation, confidence in communicating with one’s provider, and feeling prepared for decision-making at the postintervention time point [2].
Though no statistically significant effects could be found related to the digital SDM intervention’s effect on working alliance, treatment satisfaction, clinical outcomes, and hope, the results from the Momentum Trial “confirm [the] hypothesis that a digital SDM tool may promote patient activation by supporting the collaborative process between patients and their providers” [2]
Monsenso CEO Thomas Lethenborg says: “The Momentum Trial shows how promising digital tools are in supporting shared decision-making. At Monsenso, we are proud to have been involved in this research project, and look forward to empowering individuals and clinicians even more on the treatment pathway”.
——————————————————————————————————————————-
About Monsenso
Monsenso is an innovative technology company offering a digital health solution used for decentralised trials, remote patient monitoring and treatment support. Our mission is to contribute to improved health for more people at lower costs by supporting treatment digitally and leveraging patient-reported outcomes data. Our solution helps optimise the treatment and gives a detailed overview of an individual’s health through the collection of outcome, adherence, and behavioural data. It connects individuals, carers, and health care providers to enable personalised treatment, remote care, and early intervention. We collaborate with health and social care, pharmaceuticals, and leading researcher worldwide in our endeavours to deliver solutions that fit into the life of patients and health care professionals. To learn more visit www.monsenso.com
References:
[1] Alguera-Lara, V., Dowsey, M., Ride, J., Kinder, S. & Castle, D. (2017). Shared decision making in mental health: the importance for current clinical practice. Australas Psychiatry, 25(6), 578-582.
[2] Vitger, T., Hjorthøj, C., Austin, S.F., Petersen, L., Tønder, E.S., Nordentoft, M. & Korsbek, L. (2022). A Smartphone App to Promote Patient Activation and Support Shared Decision-making in People With a Diagnosis of Schizophrenia in Outpatient Treatment Settings (Momentum Trial): Randomized Controlled Assessor-Blinded Trial. Journal of Medical Internet Research, 24(10), e40292.
https://www.jmir.org/2022/10/e40292
[3] Hamann, J. & Heres, S. (2014). Adapting shared decision making for individuals with severe mental illness. Psychiatric Services, 65(12), 1483-1486.
https://ps.psychiatryonline.org/doi/full/10.1176/appi.ps.201400307
[4] Waldemar, A.K., Esbensen, B.A., Korsbek, L., Petersen, L. & Arnfred, S (2019). Recovery-oriented practice: participant observations of the interactions between patients and health professionals in mental health inpatient settings. International Journal of Mental Health Nursing, 28(1), 318-329. https://onlinelibrary.wiley.com/doi/10.1111/inm.12537
[5] Korsbek, L. (n.d.). The Momentum Trial: The efficacy of using a smartphone application to support shared decision making for people with a diagnosis of schizophrenia in an outpatient treatment setting. Open Patient data Explorative Network.
https://open.rsyd.dk/OpenProjects/openProject.jsp?openNo=451&lang=da