by Thomas Lethenborg | Aug 21, 2020 | News
Quality Policy and Standards
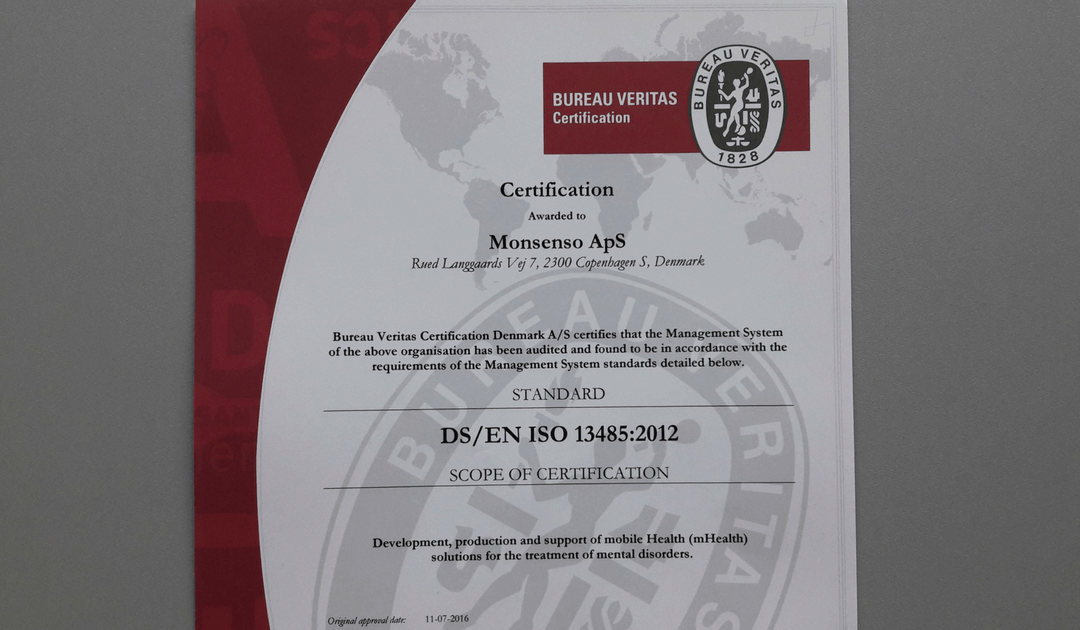
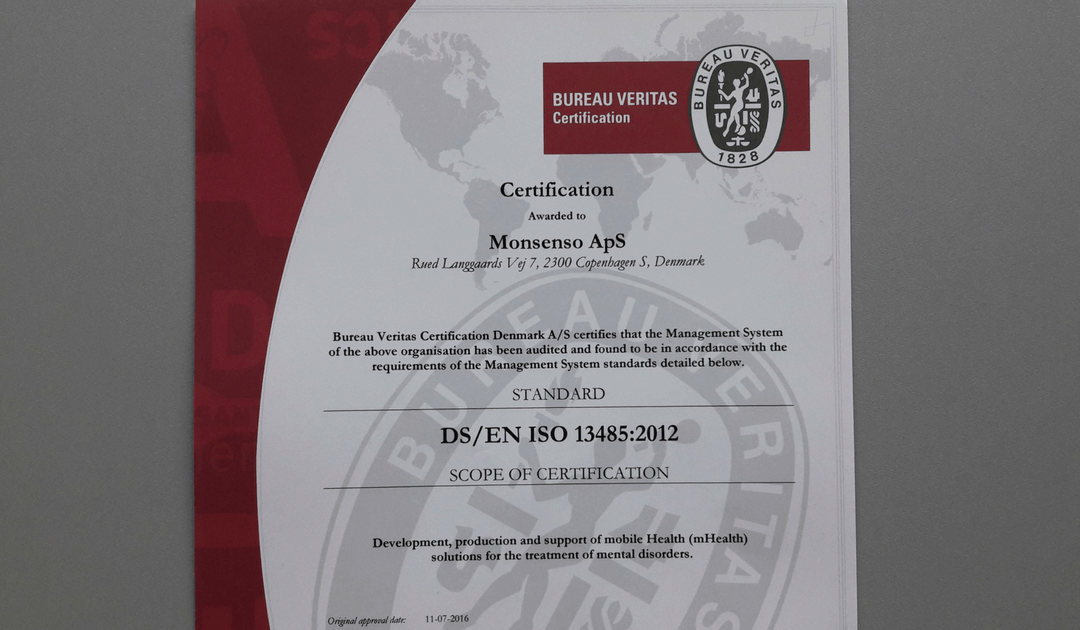
As a technology leader in mobile health (mHealth) solutions for mental health, Monsenso is ISO 13485 certified.
ISO 13485 is the gold standard for medical device companies to ensure the quality, safety and efficacy of products in the medical device field. This certification ensures that the product in question, consistently meets customer requirements and regulatory requirements applicable to medical devices and other related services.
“Monsenso adheres to the highest security standards. Beyond, being ISO 13485, Monsenso holds the ISO 27001 certifications, a TGA certification and class 1 CE mark.” says Thomas Lethenborg, CEO at Monsenso.
You can download this article as PDF in English.
For additional information contact:
Bettina van Wylich
Chief Marketing Officer
Monsenso
+45 22704724
wylich-muxoll@monsenso.com

by Thomas Lethenborg | Aug 21, 2020 | News, Press releases
Quality Policy and Standards
As a technology leader in mobile health (mHealth) solutions for mental health, Monsenso is ISO 13485 certified. ISO 13485 is the gold standard for medical device companies to ensure the quality, safety and efficacy of products in the medical device field. This certification ensures that the product in question, consistently meets customer requirements and regulatory requirements applicable to medical devices and other related services.
“Monsenso adheres to the highest security standards. Beyond, being ISO 13485 certified, Monsenso holds the ISO 27001 certification and class 1 CE mark.” says Thomas Lethenborg, CEO at Monsenso.

For additional information contact:
Jennifer Highland
Marketing and Communications Manager
Monsenso
+45 81 71 7713
highland@monsenso.com
by Thomas Lethenborg | Aug 15, 2016 | News, Press releases
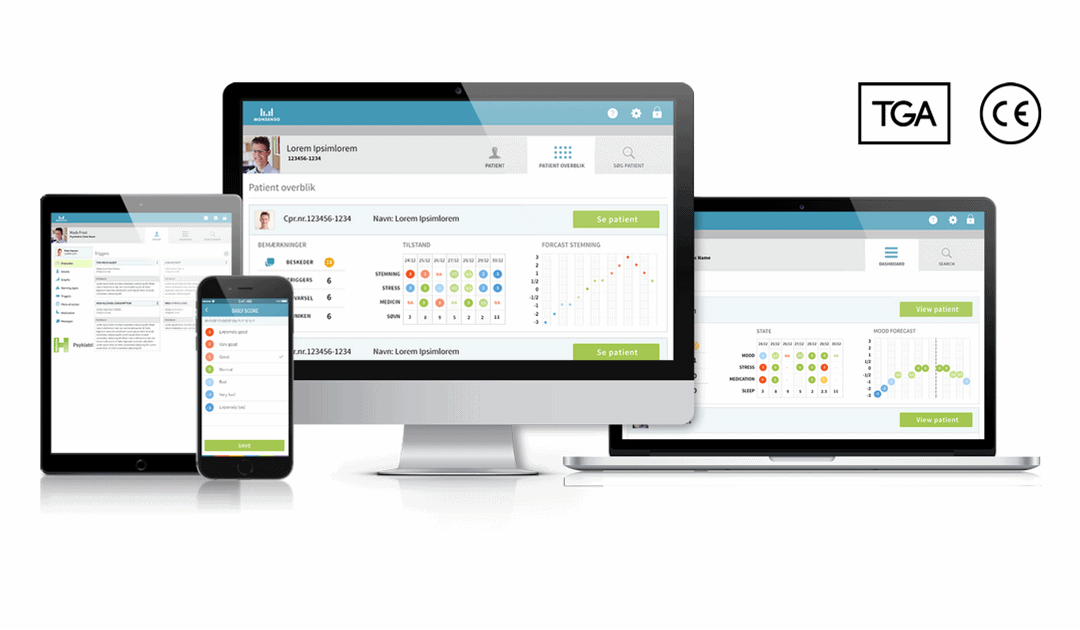
Copenhagen, Denmark – 16 August 2016. Monsenso, today announced that its mHealth solution received a Class I medical-device certification, from the Australian Register of Therapeutic Goods Administration (TGA).
The mHealth solution received the TGA certification in cooperation with Emergo, a consultancy company specialising in regulatory compliance for medical devices, with funding from the Danish Market Development Fund.
Thomas Lethenborg, CEO at Monsenso, commented “We are very satisfied that the Monsenso mHealth solution received the TGA certification and is now ready to be launched in the Australian market. Although we already have a customer in Australia, this certification provides us with the means to commercialise the solution nation-wide.”
This certification guarantees that a manufacturer’s product meets the essential requirements stipulated by the Australian Register of Terapeutic Administration.
“Holding the right certifications, and offering a high level of data security is essential for healthcare providers in all markets –including Australia. Therefore, it is important that Monsenso possesses the necessary quality control standards and adequate security measures to succeed world-wide” added Mr. Lethenborg.
The next steps for Monsenso are to obtain the ISO 13485 Certification; the ISO 27001 Data Security Certification; and to become HIPAA and FDA compliant. These certifications will be also obtained with the monetary support granted by the Danish Market Development Fund. You can download this article as PDF in English and Danish.
Note:
As of 23 May 2023, Monsenso does no longer hold the TGA certification.

by Thomas Lethenborg | Jun 21, 2016 | Blog, Mental Illness, mHealth
According to a recent statement by the new American Heart Association (AHA), major depressive disorder and bipolar disorder should be recognized as moderate risk factors for atherosclerosis and early cardiovascular disease. [1]
In 2011, the National Heart, Lung and Blood Institute identified four conditions (chronic inflammatory disease, human immunodeficiency virus, Kawasaki disease, and nephritic syndrome) that lead youths to a mild risk of developing cardiovascular disease before they reach 30. [2]
The statement released a few days ago, reveals that depression and bipolar disorder meet the same criteria as these conditions. Moreover, these two behavioural disorders are more widespread than the previous mentioned conditions combined.
These studies showed evidence of a link between paediatric depression and bipolar disorder with premature cardiovascular mortality. Cardiovascular risk factors for these teens include obesity, insulin resistance and diabetes, dyslipidemia, and hypertension.[1] According to the statement, depression and bipolar disorder are the first- and fourth-most disabling conditions, among adolescents worldwide.
After the report had been unveiled, researchers from schools around the U.S. and Canada looked at existing studies on mood disorders in people under the age of 30. Researchers looked specifically into youths suffering from depression or bipolar disorder with cardiovascular markers such as high pressure and cholesterol. They found a significant connection between having depression or bipolar disorder and increased odds of high blood pressure, high cholesterol, obesity (especially belly fat), type 2 diabetes, and hardening of the arteries. [3]
This discovery denotes that healthcare providers should track physical activity levels and food intake as well as metabolic monitoring is crucial for these young patients as a preventive measure.
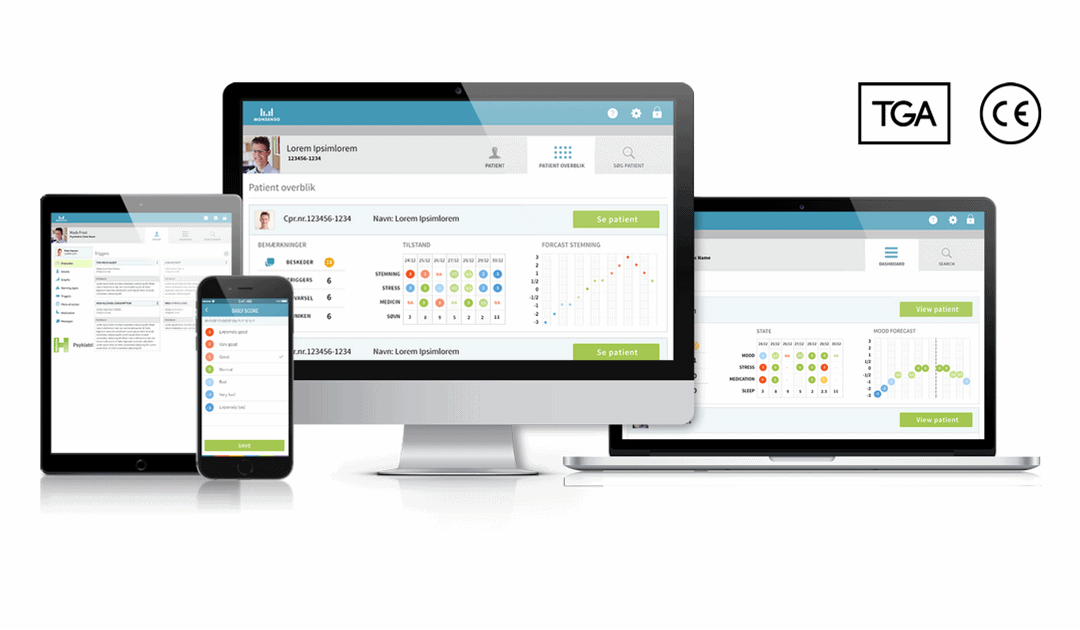
However, to monitor cardiovascular markers, physical activity and food intake, of thousands of young patients who also suffer from mental illness is not an easy task. Although, there are hundreds of smartphone applications tracking physical activity and counting calories, these apps are personal, and clinicians do not have access to an individual’s data. Nevertheless, with the Monsenso mobile health (mHealth) solution, this cumbersome task becomes easy and achievable.
The Monsenso mHealth solution enables clinicians to access a patient’s data on a daily basis. Every day, youths would be reminded to fill in a self-assessment with important information that could include the number of hours they slept, the amount of unhealthy food they have eaten, and if they realized any physical activity throughout their day. Additionally, the smartphone can also collect physical activity and mobility data, based on the smartphone’s inbuilt accelerometer and GPS locator.
The Monsenso mHealth solution, especially designed to monitor behavioural data of patients suffering from mental illness, can in this way help clinicians monitor any unhealthy habits of patients with risk of developing cardiovascular disease.
Further, with the customisable action plans, each youth could follow “contingency plans” if they experience some symptoms related to their mental illness or if they have engaged in unhealthy activities. For example, a special trigger could set up if a youth has indulged in unhealthy food for several days in a row, or has had a low level of physical activity. The action plan listed for this trigger could then encourage individuals to engage in physical activities and and to try to avoid sugar and fat during the upcoming week.
References:
[1] Browser,D Medscape. Depression, Bipolar Disorder in Teens are CVD Risk Factors: AHA (2015, August 10) http://www.medscape.com/viewarticle/849312
[2] American Heart Association. Young people with mood disorders have increased risk of developing early cardiovascular disease (2015, August 11)
http://blog.heart.org/young-people-with-mood-disorders-have-increased-risk-of-developing-early-cardiovascular-disease/
[3] Walton, A Forbes. Teens with depression, bipolar disorder, should be screened for heart disease, experts say. (2015, August 11) http://www.forbes.com/sites/alicegwalton/2015/08/11/depressed-teens-may-be-at-higher-risk-for-heart-disease/
Goldstein BI, Carnethon MR, Matthews KA, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease. Circulation 2015.

by Thomas Lethenborg | Dec 15, 2015 | mHealth, Patient Engagement
Earlier this year, Deloitte published a report titled “Connected Health: How Digital technology is transforming health and social care.” The information on this blog post has been obtained from this report.
Connected health or technology-enabled care (TEC) is the collective term used for telecare, telehealth, telemedicine, mHealth, digital health, and eHealth services. TEC is now seen as a fundamental part of the solution to solve many healthcare challenges. TEC helps people self-manage their health and well-being, alert healthcare professionals in case of any changes in an individual’s condition and support medication adherence. It also helps clinicians and care providers deliver more efficient and cost-effective care.
Digital technology is advancing exponentially, and its cost is becoming more and more affordable. At the same time, the demand for more cost-effective healthcare is rising. Now more than ever, healthcare authorities need to adopt new technologies to help meet these challenges.
An aging population
In the UK, as in other parts of the world, the population is increasing, and people are living longer. These two factors, in addition to a rise in chronic conditions, present new healthcare challenges.
Over 25% of the population in the UK are affected by a chronic condition, and an increasing number have multiple conditions. It has been appraised that people with long-term conditions use up to 50% of all GP appointments and 70% of days spent in hospital beds. It has also been estimated that their care absorbs 70% of hospital and primary care budgets in England.
Use of mobile devices is increasing amongst all age groups
Although ownership of smartphones and tablets is growing rapidly, the older population, who are the largest users of health and social care services, hadn’t adopted this technology until now. However, in 2014, baby boomers generated the fastest year-on-year growth in smartphone penetration.
Additionally, smartphone owners are encouraged to exercise, lose weight and improve their health, with the help of numerous mobile health apps.
Other market drivers
The demand for apps and wearable devices is also being driven by an increased focus on personalised care. Large pharmaceutical companies are now using apps and wearables to gather valuable health-related patient data, support their research, and provide an holistic service to patients.
In 2014, the leading pharmaceutical companies had an increase of 63 % in unique apps compared to 2013. In just one year, the total number of downloads of pharmaceutical apps increased by 197% as shown in Figure 1. These apps deliver education and training, can titrate medication and monitor compliance.
Figure 1. The number of apps published by leading pharmaceutical companies, 2013 and 2014.

There has also been an increase in on-line patient communities, using social media as a platform to exchange experiences with patients and carers.
Increasing patient trust in health apps
There is strong evidence that patients are now more than ever concerned about self-care, and they are interested in boosting their health and well-being. In addition to this, health technology companies are working to improve the quality of apps, increase user confidence and trust, and launch informed decision-making in app selection for health professionals, patients and the public.
Agencies like the US Food and Drug Administration (FDA), or NHS Choices and its NHS Health Apps Library have developed criteria that judge apps for safety and technical proficiency. For example, for apps to be included on the NHS Choices search website, which in early 2015 lists around 150 apps, they must be reviewed by a technical team (testing relevance, legal compliance and data protection), then by a clinical team (to test scientific rigour).
PatientView is an independent organisation that has developed a systematic method of appraising health apps. Until April 2015, there were 363 apps recommended for the Apple platform and 236 for Android, with smaller numbers recommended for use on other platforms.
In 2014, PatientView undertook a survey of 1,130 patient group members to identify what people want from health apps as shown in Figure 2.
Figure 2. What do patients and carers want from health apps?

Reference:
Connected Health: How Digital technology is transforming health and social care. Deloitte Health. http://www2.deloitte.com/content/dam/Deloitte/uk/Documents/life-sciences-health-care/deloitte-uk-connected-health.pdf