Patients will help document treatment efficacy in innovative, decentralised trials project
In collaboration with leading researchers and the pharmaceutical industry, the PhaseV innovation project will set new standards for how the effects of treatment can be documented so that patients are offered the right treatment. Patients and healthcare professionals will thus provide data that can help shed light on whether the treatment is working when Monsenso’s digital platform is used to support decentralised trials in the project.
To date, medical treatments have been tested primarily in long-term, randomised clinical trials to determine treatment effects and side-effects, with limited measurement of long-term effects when treatment is provided in clinical practice.
Often, drug trials take 6-15 years before a new drug can be released on the market, and 80 percent of trials fail to recruit and retain a sufficient number of patients in the trials within the set timeframe. This means that the benefits for patients and healthcare systems are often delayed. However, with digital developments, it is possible for clinics, hospitals, and patients alike to play a more active role in documenting the impact of treatments.
The new PhaseV (Phase five) innovation project, in which Innovation Fund Denmark is investing DKK 24 million (of which DKK 8,3 million goes to Monsenso), aims to develop and validate a scalable digital platform for efficient, decentralised patient recruitment, patient data collection and study execution. This is done by engaging patients and clinicians in the monitoring of treatment effects over longer periods of time based on patients’ own feedback, digital biomarkers from smartphones and wearables, as well as registry data.
“With this project, we want to show that it is possible to engage and motivate patients and healthcare professionals to collect continuous data from patients over time. PhaseV will set new standards for how the efficacy and safety of new treatments can be documented in a scalable way in the future, so that patients are offered the right treatment“, says Thomas Lethenborg, CEO of Monsenso.
“Digitizing the effect of patient treatments can be of decisive importance for our insight into the effects of the treatment of severely overweight people as well as for future clinical studies, where the goal is to make it easier for both patients and healthcare personnel to participate“, says Daniel Vega Møller, Vice President Medical & Science Obesity, NASH and Devices Novo Nordisk A/S.
Country Manager for Novartis in Denmark, Peter Drøidal, also sees great potential in the PhaseV project: “The healthcare system lacks resources and therefore we all need to think in new ways. This project’s combination of public and private partners offers unique opportunities to develop new digital solutions that can help improve patient care and free up personnel time“.
Severe obesity, urticaria and diabetic foot ulcers
The PhaseV project will develop a platform with three apps to collect data on patients with severe obesity, diabetic foot ulcers and urticaria – all of which are costly chronic conditions. For example, annual treatment costs for severe obesity alone are estimated to exceed DKK 15 billion for Danish municipalities and regions.
“More than 800,000 Danes live with severe obesity, and associated diseases are very common. As severe obesity causes both direct and indirect costs to society, there is a significant need for good and well-documented weight loss treatments“, says Jens Meldgaard Bruun, clinical professor at Aarhus University and Steno Diabetes Center Aarhus and part of PhaseV.
Urticaria affects 15-20 percent of the population, and in about 1 percent it occurs chronically and causes a severely reduced quality of life.
“Thorough monitoring and efficient data collection on symptom development are crucial for correct and effective future treatment“, says Simon Francis Thomsen, Professor and Chief Physician at Bispebjerg Hospital.
22.000 Danes live with diabetic foot ulcers and treatment costs society more than DKK 5 billion annually.
“For a patient with diabetes, a foot ulcer can become critical within days, and in exceptional cases amputation may be necessary. Hence, time is of the essence, and we want to prevent serious complications“, says Klaus Kirketerp-Møller, senior physician at Bispebjerg Hospital and Steno Diabetes Center Copenhagen.
The PhaseV project is expected to bring value to patients, regions, and municipalities, as well as to the institutions and companies involved.
Attractive new market opportunity for Monsenso
“We are further developing Monsenso’s digital health platform to improve the support of decentralised trials across chronic conditions, where behaviour and ongoing follow-up play a major role in patients’ quality of life. We see both the development work and the partnerships as very interesting for Monsenso, because it opens up a new, attractive market opportunity“, says the CEO of Monsenso, Thomas Lethenborg.
The consortium behind the project, which is supported by the Innovation Fund, includes Novo Nordisk, Novartis, Aarhus University, the Research Unit for General Practice, Aarhus Municipality, Bispebjerg Hospital, the Danish Technological Institute, the Danish Life Science Cluster, Steno Diabetes Center Aarhus, the Copenhagen Institute for Future Studies and Monsenso.
Financial expectations
The project does not change Monsenso’s financial expectations for H2 2022 but is expected to contribute to increased growth in 2023 and beyond.
Facts
Innovation Fund investment: DKK 24.3 million (of which DKK 8.3 million is for Monsenso).
Total project budget: DKK 48.2 million.
Duration: 3 years
Official title: PhaseV
Further information
CEO, Monsenso
Thomas Lethenborg
Tel. +45 21 29 88 27
E-mail: lethenborg@monsenso.com
Chairman of the board, Monsenso
Peter Mørch Eriksen
Tel. +45 29 00 35
E-mail: petermorcheriksen@outlook.com
Certified Adviser, Monsenso
Norden CEF A/S
John Norden
Tel. +45 20 72 02 00
E-mail: jn@nordencef.dk
——————————————————————————————————————————-
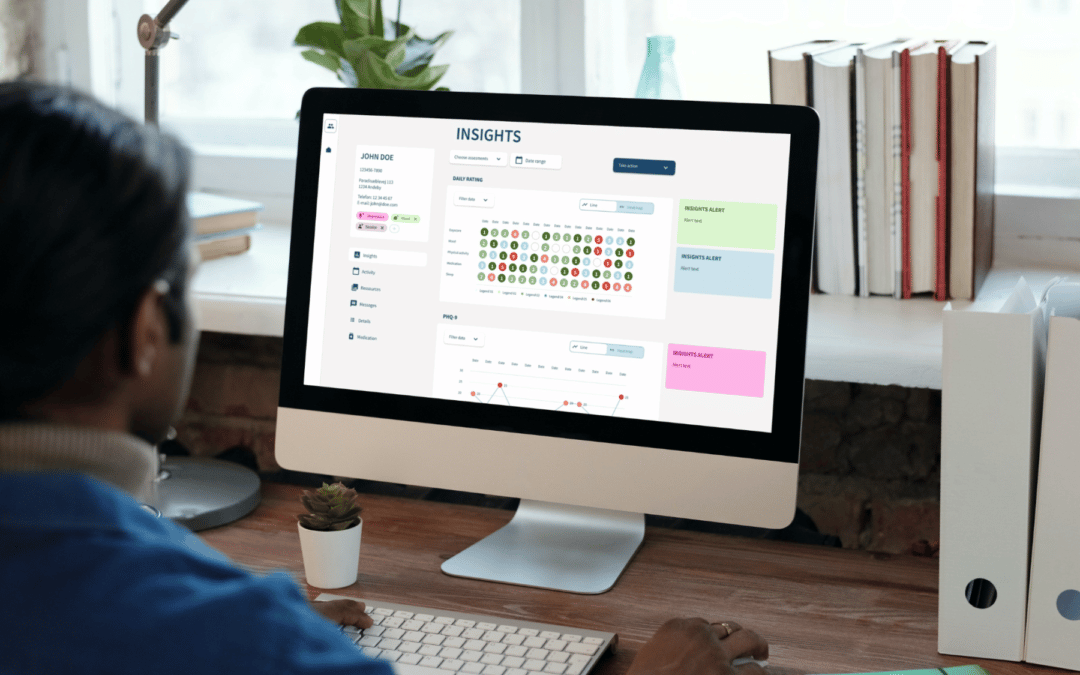
About Monsenso
Monsenso is an innovative technology company offering a digital health solution used for decentralised trials, remote patient monitoring and treatment support. Our mission is to contribute to improved health for more people at lower costs by supporting treatment digitally and leveraging patient-reported outcomes data. Our solution helps optimise the treatment and gives a detailed overview of an individual’s health through the collection of outcome, adherence and behavioural data. It connects individuals, carers and health care providers to enable personalised treatment, remote care and early intervention. We collaborate with health and social care, pharmaceuticals and leading researcher worldwide in our endeavours to deliver solutions that fit into the life of patients and health care professionals. To learn more visit www.monsenso.com