by Thomas Lethenborg | Jan 17, 2022 | Blog
Monsenso A/S, a technology leader in digital health solutions for mental health is HIPAA compliant. The Monsenso digital health solution that connects individuals and clinicians to provide optimal care adheres to the highest standards for data security and privacy. In addition to being HIPAA compliant, Monsenso holds ISO 13485 and ISO 27001 certifications, Cyber Essentials certification, a TGA certification and class 1 CE mark.
The Health Insurance Portability and Accountability Act of 1996 (HIPAA) was enacted by the U.S. Department of Health and Human Services (HHS) and is a federal law that mandates the creation of national standards to protect patients’ sensitive health information from disclosure without their consent or knowledge.
To read more about our data protection, download our Data management & Security fact sheet.
About Monsenso
Monsenso is an innovative technology company offering a digital health solution. Our mission is to help provide better mental health to more people at lower costs. Our solution helps optimise the treatment of mental disorders and gives a detailed overview of an individual’s mental health through the collection of outcome, adherence and behavioural data. It connects individuals, carers and health care providers to enable personalised treatment, remote care and early intervention. Based on continuous research and development, our team is committed to developing solutions that fit seamlessly into the lives of individuals, increase their quality of life and improve the efficacy of mental health treatment. To learn more visit www.monsenso.com.
For additional information contact:
Bettina van Wylich-Muxoll
Chief Marketing Officer
Monsenso
+45 22 70 47 24
marketing@monsenso.com
by Thomas Lethenborg | Oct 11, 2021 | News
Monsenso signs a contract with the Centre for Social Psychiatry and Substance Abuse in the municipality of Aabenraa in Denmark. The Monsenso digital health solution will be integrated as part of the treatment of citizens living in supported housing to help reduce relapses and re-admissions.
To reduce relapses and re-admissions of citizens suffering from mental disorders and substance abuse, the Centre for Social Psychiatry in Aabenraa Municipality has decided to offer the Monsenso digital health solution as an integrated part of their services in supported housing.
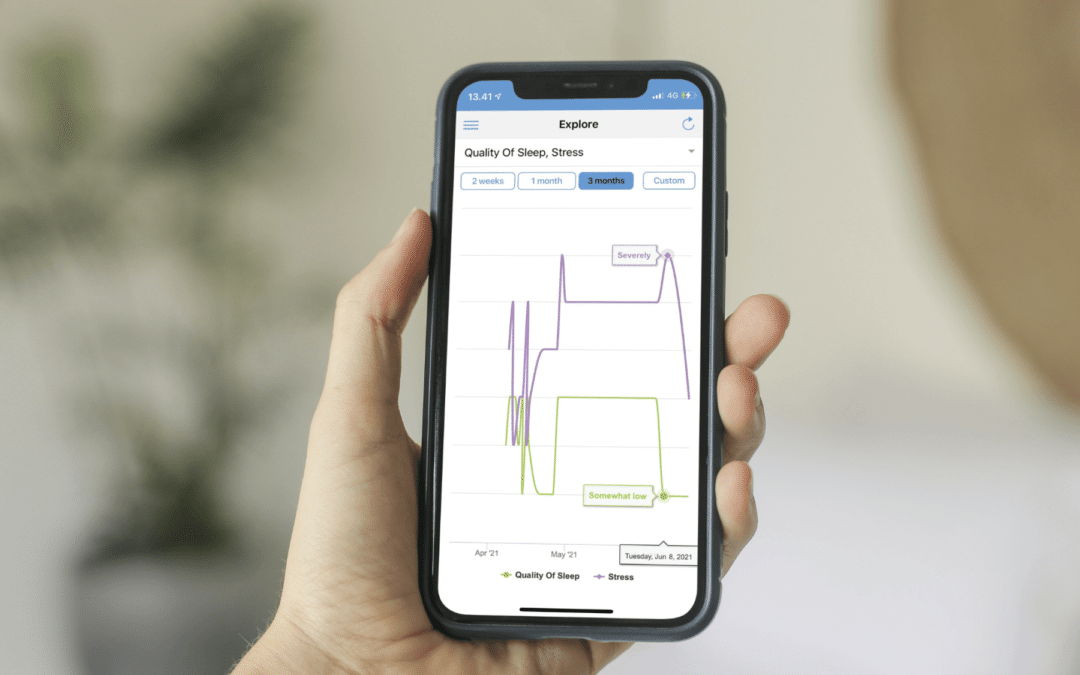
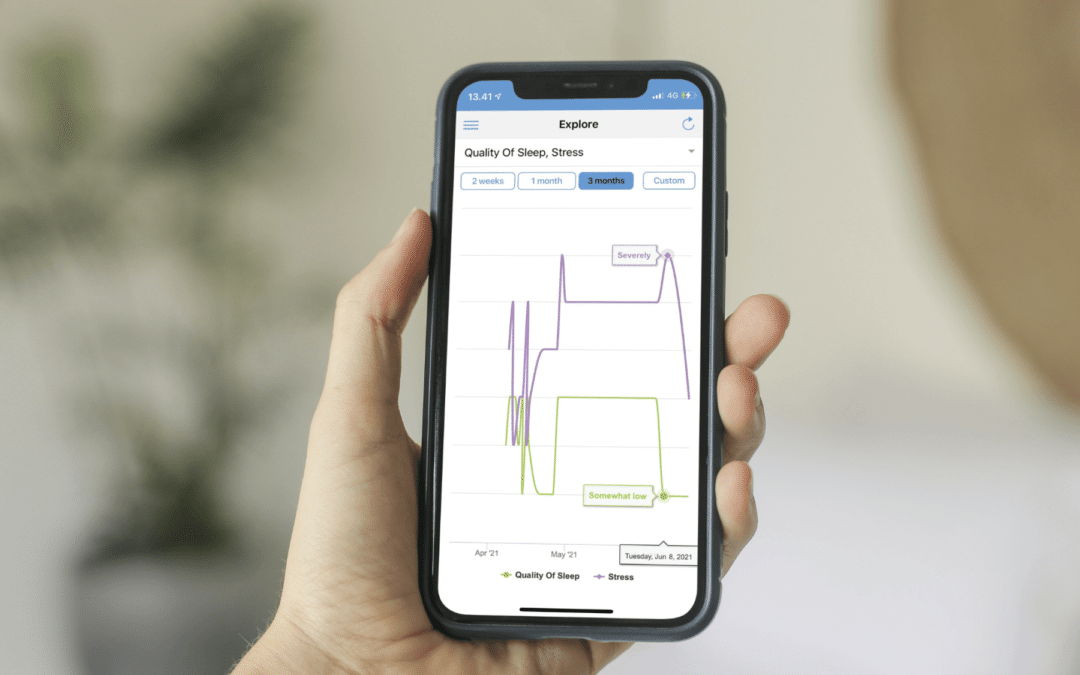
The citizens will be provided with the Monsenso app to keep track of their well-being, symptoms, and medication intake through self-reported data, as well as their behaviour through sensor data collected on mobile phones, sleep mats and watches. The historical data is visualised and helps the citizens remember how they have been doing when they speak with the housing support staff and gain better insight into the behaviours that trigger their symptoms, empowering them to better manage their condition.
The housing support staff access the data via a web portal enabling them to see fluctuations in the mental state of the citizens, hereby offering the opportunity to predict relevant outcomes for mood disorders and reduce potential relapses and readmissions.
The Monsenso app also provides treatment support in the form of Tools & Challenges and Action Plans for coping strategies that citizens can use to overcome stress and abandonment related to daily tasks.
“We are very excited about this project because the solution helps individuals take a more active role in their recovery process. The data captured provides the individuals with insight on how their lifestyle affects their mental well-being, empowering them to make positive changes” says Henning Iversen, Head of Housing Services at Aabenraa Municipality.
“We are excited to see Monsenso digital health solution integrated into the care of citizens living in supported housing.” said Thomas Lethenborg, CEO of Monsenso. “We know that one of the most important components to reducing relapse and increasing mental wellbeing is having the tools to better manage your condition”.
For additional information contact:
Bettina van Wylich-Muxoll
Chief Marketing Officer
marketing@monsenso.com
Monsenso

by Thomas Lethenborg | Jan 5, 2016 | mHealth, Patient Engagement
On the previous blog post, “Transforming health and social care with digital technology” connected health or technology-enabled care (TEC) was defined as the collective term used for telecare, telehealth, telemedicine, mHealth, digital health, and eHealth services. This type of technology can empower patients and carers by giving them more control over their health and social care needs. It can also help individuals to obtain more information regarding their health.
In broad terms, TEC can:
- Improve self-management through remote monitoring, education, and treatment adherence
- Tackle areas of unmet needs that traditional treatment struggles to address, such as mental health
- Supports the development of online patient portals and patient communities
- Transforms the relationship between patients, carers and healthcare providers to focus on co-creation
Enables self-management
Nowadays, patients and their carers use technology to research information online, identify treatment options, rate providers, and share their experiences. Healthcare needs to acknowledge that emerging technologies offer a tremendous opportunity to transform the way people engage with their health.
Besides connecting patients and providers, digital technology leads to better outcomes and a more personalised service by educating patients in regards to their health-related issues, enabling remote monitoring, and supporting treatment adherence.
Informs and educates patients and carers
It is estimated that 75% of the UK population goes online for health information. Websites, apps, videos, texts and free online courses are being used to educate and provide information to patients and their family caregivers [1].
Figure 1 displays the most common category of mobile apps: fitness, medical reference and wellness apps, which provide information with other very limited functionalities.
Figure 1. Digital health app category, percentage share in 2014.

The use of digital technology to educate patients and carers is a crucial driver of patient engagement. Surveys suggest that patients are more likely to make better choices and be engaged in their health if they can access information quickly.
Digital technology connects patients and providers, leading to better health outcomes and a more convenient and personalised service, through informing/educating, two-way remote monitoring, and supporting treatment adherence [2].
TEC can help carers understand and support those they care for by:
- Providing psychological reassurance
- Enabling carers to co-ordinate their work-life-care balance through supporting flexible hours and remote working patterns (approximately 2.3 million people have had to give up work to become carers and three million have reduced their hours)
- Delivering peer-to-peer support
Facilitates remote patient monitoring (RPM)
Remote monitoring uses technology to monitor changes in patients’ health status outside conventional clinical settings.
Historically, it allows a patient to use a device to perform a routine test and send the test data to a healthcare provider. Initially, it depended on a healthcare provider recommending its use to patients. However, digital technology has increased the potential for remote monitoring and, with the advent of apps and wearables, patients are increasingly bringing the innovation to doctors [3].
New advances in the development of biosensing wearables are spreading their capability beyond simply tracking activity. New devices can monitor a broad range of physiology (from posture to brain activity) and convert this information into outputs, through advanced connectivity and computing power.
Biosensing wearables can support people with chronic conditions, automating monitoring and detecting real time changes in an individual’s health status. Data from biosensing wearables can be uploaded to an Electronic Patient Record (EPR) and this information can be used to display an overview of a patient’s medical history in real-time, supporting early diagnoses and early intervention.
If a negative change occurs, patients, family caregivers and healthcare providers can be alerted quickly, preventing emergency admissions.
Increases treatment adherence
In bad cases, failure to follow treatment can cause a patient’s condition to deteriorate, leading to an increased likelihood of hospital admission, permanent disability, or death. Electronic reminders and alerts, via text SMS or apps, can remind patients to follow their treatment regimens, thus improving health outcomes.
The World Health Organisation has calculated that adherence to long-term therapies in developed countries is around 50%, and is even lower in developing countries [4].
In the UK, between one-third and half of all medicines prescribed for long-term conditions are not taken as recommended. It is estimated that the cost of unused or unwanted medicine is around 100 million GBP per annum [5].
Improved adherence allows healthcare providers and pharmaceutical companies to obtain a better understanding of the impact of drugs, including any complications or drug interactions, providing useful data for research. An increasing number of pharmaceutical companies are investing in digital TEC projects to increase patient adherence to the drugs they produce. Likewise, patients and carers are increasingly using digital health software to register and monitor medication intake [6].
References:
[1] Valuing Carers 2011: calculating the value of carers’ support, Carers UK and academics at the University of Leeds, May 2011.
http://circle.leeds.ac.uk/files/2012/08/110512-circle-carers-uk-valuing-carers.pdf
[2] Putting patients first. The NHS England business plan for 2013/14 and 2015/16. https://www.england.nhs.uk/wp-content/uploads/2013/04/ppf-1314-1516.pdf
[3] Primary care working differently: Telehealth and telecare –a game changer for health and social care, Deloitte UK Centre for Health Solutions, December 2012. http://www2.deloitte.com/content/dam/Deloitte/uk/Documents/life-sciences-health-care/deloitte-uk-telehealth-telecare.pdf
[4] Medication Adherence: WHO Cares? Mayo Clinic 2011. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3068890/
[5] Aston Medication Adherence Study, Aston University. See also: http://www.aston.ac.uk/lhs/research/health/pharmacy/adherence/
[6] Mobile apps, fighting for patient adherence, Mobile health global, December 2014. See also http://www.mobilehealthglobal.com/in-the-news/news/109/mobile-apps-fighting-for-patient-adherence
[7] Psychological Therapies, Annual Report on the use of IAPT services: England – 2013/14 Experimental Statistics, Health and Social Care Information Centre, September 2014. http://www.hscic.gov.uk/catalogue/PUB14899/psyc-ther-ann-rep-2013-14.pdf

by Thomas Lethenborg | Dec 15, 2015 | mHealth, Patient Engagement
Earlier this year, Deloitte published a report titled “Connected Health: How Digital technology is transforming health and social care.” The information on this blog post has been obtained from this report.
Connected health or technology-enabled care (TEC) is the collective term used for telecare, telehealth, telemedicine, mHealth, digital health, and eHealth services. TEC is now seen as a fundamental part of the solution to solve many healthcare challenges. TEC helps people self-manage their health and well-being, alert healthcare professionals in case of any changes in an individual’s condition and support medication adherence. It also helps clinicians and care providers deliver more efficient and cost-effective care.
Digital technology is advancing exponentially, and its cost is becoming more and more affordable. At the same time, the demand for more cost-effective healthcare is rising. Now more than ever, healthcare authorities need to adopt new technologies to help meet these challenges.
An aging population
In the UK, as in other parts of the world, the population is increasing, and people are living longer. These two factors, in addition to a rise in chronic conditions, present new healthcare challenges.
Over 25% of the population in the UK are affected by a chronic condition, and an increasing number have multiple conditions. It has been appraised that people with long-term conditions use up to 50% of all GP appointments and 70% of days spent in hospital beds. It has also been estimated that their care absorbs 70% of hospital and primary care budgets in England.
Use of mobile devices is increasing amongst all age groups
Although ownership of smartphones and tablets is growing rapidly, the older population, who are the largest users of health and social care services, hadn’t adopted this technology until now. However, in 2014, baby boomers generated the fastest year-on-year growth in smartphone penetration.
Additionally, smartphone owners are encouraged to exercise, lose weight and improve their health, with the help of numerous mobile health apps.
Other market drivers
The demand for apps and wearable devices is also being driven by an increased focus on personalised care. Large pharmaceutical companies are now using apps and wearables to gather valuable health-related patient data, support their research, and provide an holistic service to patients.
In 2014, the leading pharmaceutical companies had an increase of 63 % in unique apps compared to 2013. In just one year, the total number of downloads of pharmaceutical apps increased by 197% as shown in Figure 1. These apps deliver education and training, can titrate medication and monitor compliance.
Figure 1. The number of apps published by leading pharmaceutical companies, 2013 and 2014.

There has also been an increase in on-line patient communities, using social media as a platform to exchange experiences with patients and carers.
Increasing patient trust in health apps
There is strong evidence that patients are now more than ever concerned about self-care, and they are interested in boosting their health and well-being. In addition to this, health technology companies are working to improve the quality of apps, increase user confidence and trust, and launch informed decision-making in app selection for health professionals, patients and the public.
Agencies like the US Food and Drug Administration (FDA), or NHS Choices and its NHS Health Apps Library have developed criteria that judge apps for safety and technical proficiency. For example, for apps to be included on the NHS Choices search website, which in early 2015 lists around 150 apps, they must be reviewed by a technical team (testing relevance, legal compliance and data protection), then by a clinical team (to test scientific rigour).
PatientView is an independent organisation that has developed a systematic method of appraising health apps. Until April 2015, there were 363 apps recommended for the Apple platform and 236 for Android, with smaller numbers recommended for use on other platforms.
In 2014, PatientView undertook a survey of 1,130 patient group members to identify what people want from health apps as shown in Figure 2.
Figure 2. What do patients and carers want from health apps?

Reference:
Connected Health: How Digital technology is transforming health and social care. Deloitte Health. http://www2.deloitte.com/content/dam/Deloitte/uk/Documents/life-sciences-health-care/deloitte-uk-connected-health.pdf

by Thomas Lethenborg | Dec 8, 2015 | mHealth
Early intervention is critical to treating mental illness before it can cause tragic results such as serious impairment, unemployment, homelessness, poverty, and suicide [1].
The identification of mental illness and its treatment, as early as possible, represents a high priority. The early detection and treatment of mental illness promote recovery, independence, and self-sufficiency, as well as facilitating social activities and employment opportunities [2].
It is estimated that 100,000 adolescents and young adults in the United States alone experience a first episode of psychosis every year. The early phase of psychotic illness is widely viewed as a critical opportunity for indicated prevention, and a chance to alter the downward trajectory and poor outcomes associated with serious mental disorders such as schizophrenia. The timing of treatment is critical; short and long-term outcomes are better when individuals begin treatment close to the onset of psychosis. Numerous studies find a substantial delay between the onset of psychotic symptoms and the initiation of treatment. In the U.S., treatment is typically delayed between one and three years, suggesting that many people experiencing first episodes of psychosis are missing a critical opportunity to benefit from early intervention [3].
Early identification and rapid referral are essential to shortening the duration of untreated psychosis and pre-empting functional deterioration. The World Health Organization advocates reducing the duration of untreated psychosis to three months or less by addressing “bottlenecks” in the pathway from early psychosis identification to initiation of specialty care [3].
To support early intervention, in 2009, the National Institute of Mental Health (NIMH), implemented a research project to change the prognosis of schizophrenia through aggressive treatment in the earliest stages of illness.Recovery After an Initial Schizophrenia Episode (RAISE) is designed to reduce the likelihood of long-term disability that people with schizophrenia often experience. It aims to help people with the disorder lead productive, independent lives. At the same time, it aims to reduce the financial impact on the public systems often tapped to pay for the care of people with schizophrenia [4].
In 2011, RAISE began conducting a full-scale, randomized controlled trial comparing two different ways of providing treatment to people experiencing the early stages of schizophrenia and related disorders. Both types of treatment emphasize early intervention but feature different approaches for initiating and coordinating care. Treatment may include personalized medication treatment, individual resiliency training, and supportive services, such as family psychoeducation and education or employment assistance [5]. The RAISE study, expected to be completed by August 2016, aims to emphasize the importance of early intervention.
The Monsenso mHealth solution can help healthcare providers to closely monitor patients who have experienced a first episode of mental illness.
After experiencing a first episode, the healthcare provider can encourage the patient to use the Monsenso mHealth solution. This will enable the clinician to monitor the individual on a continuous basis, and react if symptoms arise.
With the Monsenso user app, patients can fill in self-assessments on a daily basis. These self-assessments include information on the patient’s behaviour and symptoms related to his mental health. Furthermore, the solution collects sensor data through sensors in the patient’s smartphone, and this combined with the self-assessment will help the healthcare provider to continuously monitor the patient, and support intervention at a very early stage. Early warning signs and automatic triggers can be set to indicate to the health care provider that proactive intervention is needed, if for example a patient sleeps too little or feels too distressed.
Early intervention and continuous monitoring can maximize a person’s chances of a fast recovery, self-sufficiency, and living a high-quality life including the possibility to pursue and education and maintain a stable job.
References:
[1] Directors Blog: SAMHSA and NIMH partner to support early intervention for serious mental illness. P. Hyde and T. Insel. National Institute of Mental Health Blog (2014, June 17) http://www.nimh.nih.gov/about/director/2014/samhsa-and-nimh-partner-to-support-early-intervention-for-serious-mental-illness.shtml
[2] Early intervention and recovery for young people with early psychosis: consensus statement. J. Bertolote and P. McGorry. British Journal of Psychiatry (2005). http://bjp.rcpsych.org/content/bjprcpsych/187/48/s116.full.pdf
[3] Evidence based treatment for first episode of psychosis: Components of coordinated specialty care. PHD R. K. Heinssen. RAISE NIMH (2014, April 14). http://www.nimh.nih.gov/health/topics/schizophrenia/raise/nimh-white-paper-csc-for-fep_147096.pdf
[4] Raise Project Overview. National Institute of Mental Health. (2009)http://www.nimh.nih.gov/health/topics/schizophrenia/raise/index.shtml
[5] NIMH RAISE Project makes progress as team refines research approach. National Institute of Mental Health. (2011, August 9) http://www.nimh.nih.gov/news/science-news/2011/nimh-raise-project-makes-progress-as-teams-refine-research-approaches.shtml