Healthier together – The EU Non-Communicable Diseases Initiative
Did you know that every year, 41 million people die from non-communicable diseases (71% of all deaths worldwide) and that over 15 million people out of those are only aged 30-69 [1]?
Non-communicable diseases (NCDs) are defined as chronic health conditions that have “genetic, lifestyle, or environmental causes rather than viral or bacterial” ones [2]. NCDs are not contagious, but they do result in long-term health issues and often require long-term treatment and care [2]. Apart from diseases such as cancer or diabetes, mental disorders also fall into the category of non-communicable diseases [1].
In a previous blog post, we explored approaches taken to improve mental health in Denmark. But what are we actually doing on an EU level to ease the burden of mental illness on our international societies?
The EU Non-Communicable Diseases Initiative
In order to fight non-communicable diseases and support the people suffering from them, the European Commission has launched the Healthier together – EU Non-Communicable Diseases Initiative (EU NCD Initiative), aimed at covering the period from 2022 to 2027. The main objective of this initiative is “to support EU countries in identifying and implementing effective policies and actions to reduce the burden of major non-communicable diseases (NCDs) and improve citizens’ health and well-being.” [3].
One of the five strands covered by the initiative is mental health and neurological disorders.
The EU NCD Initiative aims at mental health and well-being promotion, improved prevention and treatment of mental disorders, and better support for individuals suffering from mental health problems. In order to accomplish this, a need for setting up improved “supportive structures, mechanisms and processes for integrated policies and actions to support mental health” has been defined [3].
Collaborative action on mental health and neurological disorders
The European Commission has suggested several “work packages” on mental health and neurological disorders, with the goal to reduce the burden of mental illness on our international society. Possible priority areas defined include:
- Adopting a mental health-in-all-policies approach: Overall creation of favourable conditions addressing environmental and social determinants for better mental health
- Focusing on mental health promotion and mental illness prevention, e.g. by supporting “the development of social and emotional skills in childhood” [3] and by preventing burnout and stress at the workplace
- Improving the provision of access to high-quality mental health services, e.g. by increasing the capacity in order to meet the growing need for mental health support
- Tackling stigma against mental health conditions and enhancing the social inclusion of individuals suffering from poor mental health
Digitalization needs to become a priority
According to Dr Hans Henri P. Kluge, WHO Regional Director for Europe, “personnel shortages [and] insufficient recruitment and retention […] are blighting health systems” [4].
While the need to hire more trained professionals is undoubtedly critical to improve mental health services, this may also be an opportunity for scalable technologies to improve the reach of the current workforce to serve the needs of patients waiting to receive care.
Surprisingly, when being asked to indicate overall priority areas across the different strands covered by the NCD initiative, only two EU countries (specify which) endorsed “digital tools to support health promotion, disease prevention and management” as a priority area [3].
In contrast, a large study by Elsevier Health (2022) shows that 77% of international clinicians expect tech companies to become “key stakeholders in managing healthcare systems in 10 years”, and that the majority of clinicians (70%) believe an increased use of digital technologies will transform healthcare positively [5].
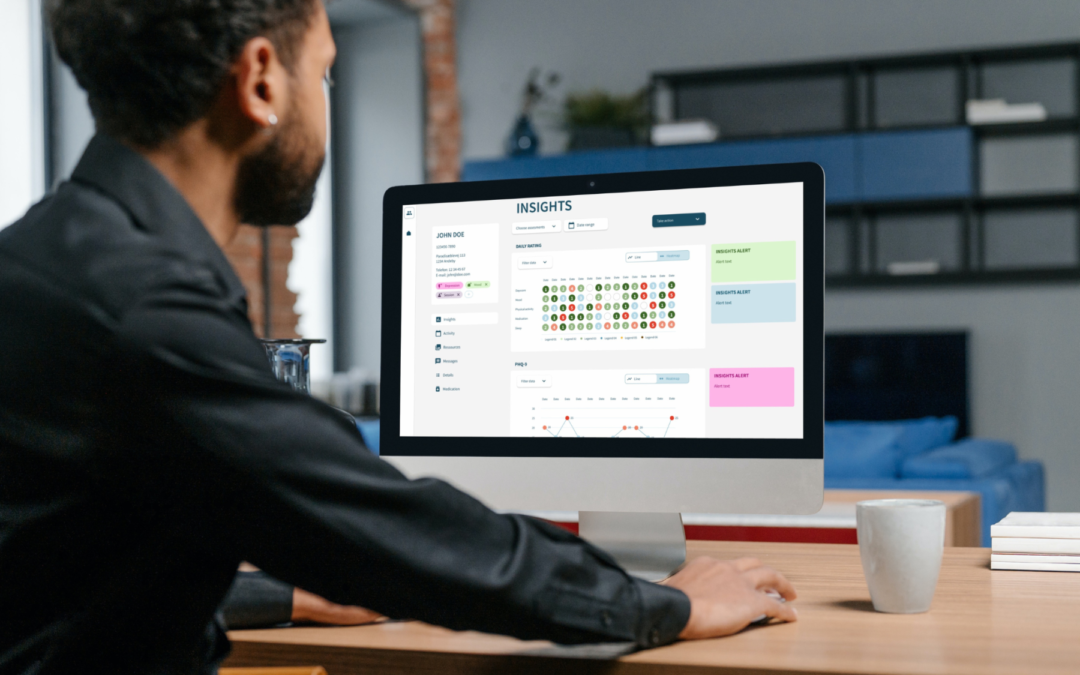
The use of digital technology offers the potential to address challenges in European mental health services. In particular, the use of digital platforms for remote patient monitoring and health assessment could improve access and speed to care, and real-time patient analytics could enable personalised treatment and improved quality of care [5].
In summary, the EU Non-Communicable Diseases Initiative has ambitious goals to provide better mental health services to more people. However, with the majority of EU countries not endorsing “digital tools to support health promotion, disease prevention and management” [3] as a priority area, raising awareness about the potential of digital health is highly important if these goals are to be achieved.
——————————————————————————————————————————-
About Monsenso
Monsenso is an innovative technology company offering a digital health solution used for decentralised trials, remote patient monitoring and treatment support. Our mission is to contribute to improved health for more people at lower costs by supporting treatment digitally and leveraging patient-reported outcomes data. Our solution helps optimise the treatment and gives a detailed overview of an individual’s health through the collection of outcome, adherence, and behavioural data. It connects individuals, carers, and health care providers to enable personalised treatment, remote care, and early intervention. We collaborate with health and social care, pharmaceuticals, and leading researcher worldwide in our endeavours to deliver solutions that fit into the life of patients and health care professionals. To learn more visit www.monsenso.com.
References:
[1] World Health Organization (2021). Noncommunicable diseases.
https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
[2] WebMD (n.d.). What Is Non-Communicable Disease?
https://www.webmd.com/a-to-z-guides/what-is-non-communicable-disease
[3] European Commission (2022). Healthier Together – EU non-Communicable Disease Initiative.
https://health.ec.europa.eu/non-communicable-diseases/healthier-together-eu-non-communicable-diseases-initiative_en
[4] World Health Organization (2022). Ticking timebomb: Without immediate action, health and care workforce gaps in the European Region could spell disaster.
https://www.who.int/europe/news/item/14-09-2022-ticking-timebomb–without-immediate-action–health-and-care-workforce-gaps-in-the-european-region-could-spell-disaster
[5] Elsevier Health (2022). Clinician of the Future Report 2022.
https://www.elsevier.com/connect/clinician-of-the-future