by Thomas Lethenborg | Jun 21, 2016 | Blog, Mental Illness, mHealth
According to a recent statement by the new American Heart Association (AHA), major depressive disorder and bipolar disorder should be recognized as moderate risk factors for atherosclerosis and early cardiovascular disease. [1]
In 2011, the National Heart, Lung and Blood Institute identified four conditions (chronic inflammatory disease, human immunodeficiency virus, Kawasaki disease, and nephritic syndrome) that lead youths to a mild risk of developing cardiovascular disease before they reach 30. [2]
The statement released a few days ago, reveals that depression and bipolar disorder meet the same criteria as these conditions. Moreover, these two behavioural disorders are more widespread than the previous mentioned conditions combined.
These studies showed evidence of a link between paediatric depression and bipolar disorder with premature cardiovascular mortality. Cardiovascular risk factors for these teens include obesity, insulin resistance and diabetes, dyslipidemia, and hypertension.[1] According to the statement, depression and bipolar disorder are the first- and fourth-most disabling conditions, among adolescents worldwide.
After the report had been unveiled, researchers from schools around the U.S. and Canada looked at existing studies on mood disorders in people under the age of 30. Researchers looked specifically into youths suffering from depression or bipolar disorder with cardiovascular markers such as high pressure and cholesterol. They found a significant connection between having depression or bipolar disorder and increased odds of high blood pressure, high cholesterol, obesity (especially belly fat), type 2 diabetes, and hardening of the arteries. [3]
This discovery denotes that healthcare providers should track physical activity levels and food intake as well as metabolic monitoring is crucial for these young patients as a preventive measure.
However, to monitor cardiovascular markers, physical activity and food intake, of thousands of young patients who also suffer from mental illness is not an easy task. Although, there are hundreds of smartphone applications tracking physical activity and counting calories, these apps are personal, and clinicians do not have access to an individual’s data. Nevertheless, with the Monsenso mobile health (mHealth) solution, this cumbersome task becomes easy and achievable.
The Monsenso mHealth solution enables clinicians to access a patient’s data on a daily basis. Every day, youths would be reminded to fill in a self-assessment with important information that could include the number of hours they slept, the amount of unhealthy food they have eaten, and if they realized any physical activity throughout their day. Additionally, the smartphone can also collect physical activity and mobility data, based on the smartphone’s inbuilt accelerometer and GPS locator.
The Monsenso mHealth solution, especially designed to monitor behavioural data of patients suffering from mental illness, can in this way help clinicians monitor any unhealthy habits of patients with risk of developing cardiovascular disease.
Further, with the customisable action plans, each youth could follow “contingency plans” if they experience some symptoms related to their mental illness or if they have engaged in unhealthy activities. For example, a special trigger could set up if a youth has indulged in unhealthy food for several days in a row, or has had a low level of physical activity. The action plan listed for this trigger could then encourage individuals to engage in physical activities and and to try to avoid sugar and fat during the upcoming week.
References:
[1] Browser,D Medscape. Depression, Bipolar Disorder in Teens are CVD Risk Factors: AHA (2015, August 10) http://www.medscape.com/viewarticle/849312
[2] American Heart Association. Young people with mood disorders have increased risk of developing early cardiovascular disease (2015, August 11)
http://blog.heart.org/young-people-with-mood-disorders-have-increased-risk-of-developing-early-cardiovascular-disease/
[3] Walton, A Forbes. Teens with depression, bipolar disorder, should be screened for heart disease, experts say. (2015, August 11) http://www.forbes.com/sites/alicegwalton/2015/08/11/depressed-teens-may-be-at-higher-risk-for-heart-disease/
Goldstein BI, Carnethon MR, Matthews KA, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease. Circulation 2015.

by Thomas Lethenborg | Dec 15, 2015 | mHealth, Patient Engagement
Earlier this year, Deloitte published a report titled “Connected Health: How Digital technology is transforming health and social care.” The information on this blog post has been obtained from this report.
Connected health or technology-enabled care (TEC) is the collective term used for telecare, telehealth, telemedicine, mHealth, digital health, and eHealth services. TEC is now seen as a fundamental part of the solution to solve many healthcare challenges. TEC helps people self-manage their health and well-being, alert healthcare professionals in case of any changes in an individual’s condition and support medication adherence. It also helps clinicians and care providers deliver more efficient and cost-effective care.
Digital technology is advancing exponentially, and its cost is becoming more and more affordable. At the same time, the demand for more cost-effective healthcare is rising. Now more than ever, healthcare authorities need to adopt new technologies to help meet these challenges.
An aging population
In the UK, as in other parts of the world, the population is increasing, and people are living longer. These two factors, in addition to a rise in chronic conditions, present new healthcare challenges.
Over 25% of the population in the UK are affected by a chronic condition, and an increasing number have multiple conditions. It has been appraised that people with long-term conditions use up to 50% of all GP appointments and 70% of days spent in hospital beds. It has also been estimated that their care absorbs 70% of hospital and primary care budgets in England.
Use of mobile devices is increasing amongst all age groups
Although ownership of smartphones and tablets is growing rapidly, the older population, who are the largest users of health and social care services, hadn’t adopted this technology until now. However, in 2014, baby boomers generated the fastest year-on-year growth in smartphone penetration.
Additionally, smartphone owners are encouraged to exercise, lose weight and improve their health, with the help of numerous mobile health apps.
Other market drivers
The demand for apps and wearable devices is also being driven by an increased focus on personalised care. Large pharmaceutical companies are now using apps and wearables to gather valuable health-related patient data, support their research, and provide an holistic service to patients.
In 2014, the leading pharmaceutical companies had an increase of 63 % in unique apps compared to 2013. In just one year, the total number of downloads of pharmaceutical apps increased by 197% as shown in Figure 1. These apps deliver education and training, can titrate medication and monitor compliance.
Figure 1. The number of apps published by leading pharmaceutical companies, 2013 and 2014.

There has also been an increase in on-line patient communities, using social media as a platform to exchange experiences with patients and carers.
Increasing patient trust in health apps
There is strong evidence that patients are now more than ever concerned about self-care, and they are interested in boosting their health and well-being. In addition to this, health technology companies are working to improve the quality of apps, increase user confidence and trust, and launch informed decision-making in app selection for health professionals, patients and the public.
Agencies like the US Food and Drug Administration (FDA), or NHS Choices and its NHS Health Apps Library have developed criteria that judge apps for safety and technical proficiency. For example, for apps to be included on the NHS Choices search website, which in early 2015 lists around 150 apps, they must be reviewed by a technical team (testing relevance, legal compliance and data protection), then by a clinical team (to test scientific rigour).
PatientView is an independent organisation that has developed a systematic method of appraising health apps. Until April 2015, there were 363 apps recommended for the Apple platform and 236 for Android, with smaller numbers recommended for use on other platforms.
In 2014, PatientView undertook a survey of 1,130 patient group members to identify what people want from health apps as shown in Figure 2.
Figure 2. What do patients and carers want from health apps?

Reference:
Connected Health: How Digital technology is transforming health and social care. Deloitte Health. http://www2.deloitte.com/content/dam/Deloitte/uk/Documents/life-sciences-health-care/deloitte-uk-connected-health.pdf
by Thomas Lethenborg | Dec 11, 2015 | mHealth
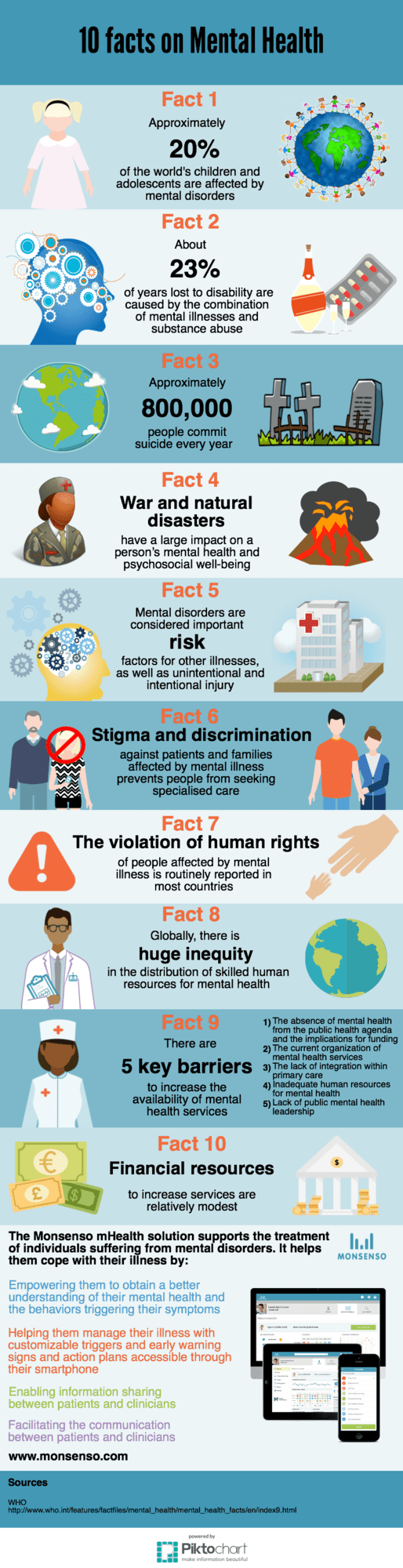
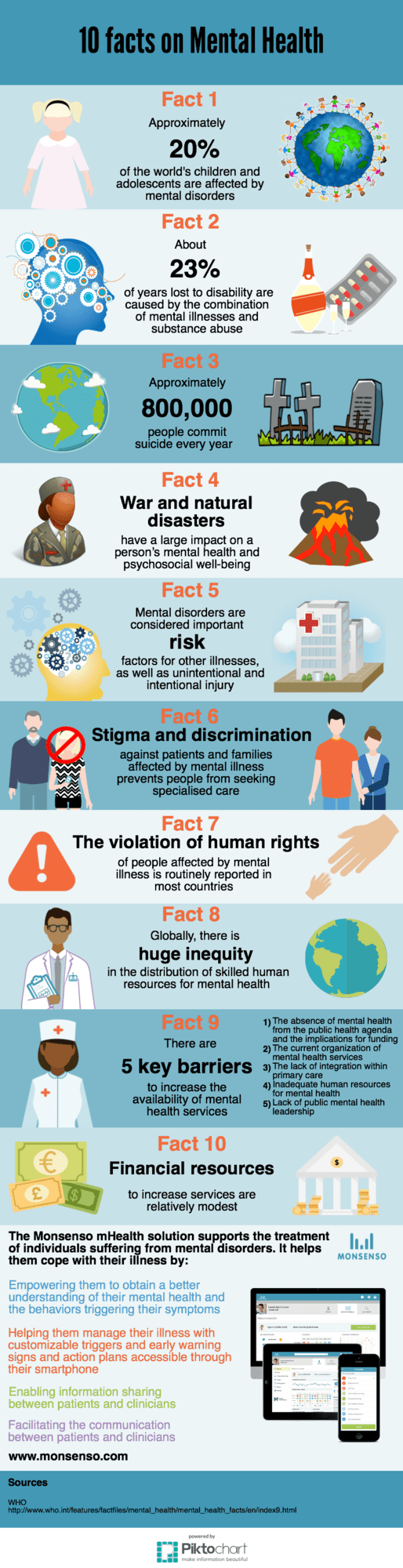
Approximately 20% of the world’s children and adolescents are affected by mental disorders. Mental illnesses and substance abuse are the leading causes of disability worldwide.

by Thomas Lethenborg | Dec 8, 2015 | mHealth
Early intervention is critical to treating mental illness before it can cause tragic results such as serious impairment, unemployment, homelessness, poverty, and suicide [1].
The identification of mental illness and its treatment, as early as possible, represents a high priority. The early detection and treatment of mental illness promote recovery, independence, and self-sufficiency, as well as facilitating social activities and employment opportunities [2].
It is estimated that 100,000 adolescents and young adults in the United States alone experience a first episode of psychosis every year. The early phase of psychotic illness is widely viewed as a critical opportunity for indicated prevention, and a chance to alter the downward trajectory and poor outcomes associated with serious mental disorders such as schizophrenia. The timing of treatment is critical; short and long-term outcomes are better when individuals begin treatment close to the onset of psychosis. Numerous studies find a substantial delay between the onset of psychotic symptoms and the initiation of treatment. In the U.S., treatment is typically delayed between one and three years, suggesting that many people experiencing first episodes of psychosis are missing a critical opportunity to benefit from early intervention [3].
Early identification and rapid referral are essential to shortening the duration of untreated psychosis and pre-empting functional deterioration. The World Health Organization advocates reducing the duration of untreated psychosis to three months or less by addressing “bottlenecks” in the pathway from early psychosis identification to initiation of specialty care [3].
To support early intervention, in 2009, the National Institute of Mental Health (NIMH), implemented a research project to change the prognosis of schizophrenia through aggressive treatment in the earliest stages of illness.Recovery After an Initial Schizophrenia Episode (RAISE) is designed to reduce the likelihood of long-term disability that people with schizophrenia often experience. It aims to help people with the disorder lead productive, independent lives. At the same time, it aims to reduce the financial impact on the public systems often tapped to pay for the care of people with schizophrenia [4].
In 2011, RAISE began conducting a full-scale, randomized controlled trial comparing two different ways of providing treatment to people experiencing the early stages of schizophrenia and related disorders. Both types of treatment emphasize early intervention but feature different approaches for initiating and coordinating care. Treatment may include personalized medication treatment, individual resiliency training, and supportive services, such as family psychoeducation and education or employment assistance [5]. The RAISE study, expected to be completed by August 2016, aims to emphasize the importance of early intervention.
The Monsenso mHealth solution can help healthcare providers to closely monitor patients who have experienced a first episode of mental illness.
After experiencing a first episode, the healthcare provider can encourage the patient to use the Monsenso mHealth solution. This will enable the clinician to monitor the individual on a continuous basis, and react if symptoms arise.
With the Monsenso user app, patients can fill in self-assessments on a daily basis. These self-assessments include information on the patient’s behaviour and symptoms related to his mental health. Furthermore, the solution collects sensor data through sensors in the patient’s smartphone, and this combined with the self-assessment will help the healthcare provider to continuously monitor the patient, and support intervention at a very early stage. Early warning signs and automatic triggers can be set to indicate to the health care provider that proactive intervention is needed, if for example a patient sleeps too little or feels too distressed.
Early intervention and continuous monitoring can maximize a person’s chances of a fast recovery, self-sufficiency, and living a high-quality life including the possibility to pursue and education and maintain a stable job.
References:
[1] Directors Blog: SAMHSA and NIMH partner to support early intervention for serious mental illness. P. Hyde and T. Insel. National Institute of Mental Health Blog (2014, June 17) http://www.nimh.nih.gov/about/director/2014/samhsa-and-nimh-partner-to-support-early-intervention-for-serious-mental-illness.shtml
[2] Early intervention and recovery for young people with early psychosis: consensus statement. J. Bertolote and P. McGorry. British Journal of Psychiatry (2005). http://bjp.rcpsych.org/content/bjprcpsych/187/48/s116.full.pdf
[3] Evidence based treatment for first episode of psychosis: Components of coordinated specialty care. PHD R. K. Heinssen. RAISE NIMH (2014, April 14). http://www.nimh.nih.gov/health/topics/schizophrenia/raise/nimh-white-paper-csc-for-fep_147096.pdf
[4] Raise Project Overview. National Institute of Mental Health. (2009)http://www.nimh.nih.gov/health/topics/schizophrenia/raise/index.shtml
[5] NIMH RAISE Project makes progress as team refines research approach. National Institute of Mental Health. (2011, August 9) http://www.nimh.nih.gov/news/science-news/2011/nimh-raise-project-makes-progress-as-teams-refine-research-approaches.shtml

by Thomas Lethenborg | Dec 3, 2015 | Bipolar, mHealth
Bipolar disorder, also known as manic-depressive illness, is a brain disorder that causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks. [1]
People suffering from bipolar disorder will have periods or episodes of depression – where they feel very low and lethargic mania – where they feel high and overactive. [2]
Unlike simple mood swings, each episode of bipolar disorder can last for several weeks and some people may not experience a “normal” mood very often. [2]
Getting an accurate diagnosis is the first step in bipolar disorder treatment. However, this isn’t always easy. The mood swings of bipolar disorder can be difficult to distinguish from other problems such as major depression, ADHD, and borderline personality disorder. For many people suffering from bipolar disorder, it takes years and numerous doctor visits before the problem is correctly identified and treated. [3]
Indicators of bipolar disorder:
- Repeated episodes of major depression
- First episode of major depression was experienced before age 25
- First-degree relative suffering from bipolar disorder
- Mood and energy levels are higher than most people’s when not depressed
- Oversleeping and overeating when depressed
- Episodes of major depression are shorter than 3 months
- Lost contact with reality while depressed
- Suffered from postpartum depression in the past
- Developed mania or hypomania while taking antidepressants
- Antidepressants stopped working after several months
- Tried three or more antidepressants without success [3]
If a person is not treated, episodes of bipolar-related mania can last for between three to six months. Episodes of depression tend to last longer, for between six and twelve months. However, with effective treatment, episodes usually improve within about three months. [2]
Most people with bipolar disorder can be treated using a combination of different treatments that can include:
- Medication such as mood stabilisers and antidepressants
- Learning to recognize triggers and early warning signs of an episode of depression or mania
- Psychotherapy to deal with depression and provide advice on how to improve relationships
- Lifestyle advice such as doing regular exercise, planning activities you enjoy that give you a sense of achievement, and advice on improving your diet and getting more sleep [2]
Mobile health technology
The Monsenso mHealth platform is based on The MONARCA Research Project, aimed at developing and validating a solution for multi-parametric, long-term monitoring of behavioral and physiological information relevant to bipolar disorder.
The Monsenso solution can help predict and prevent episodes by training patients to recognize their early warning signs, which are symptoms that indicate an oncoming episode [4].
In particular, during the research project, it was discovered that these three parameters are crucial in keeping a bipolar patient stable:
- Adherence to prescribed medication: Taking all medications on a daily basis, exactly as prescribed.
- Stable sleep patterns: Sleeping eight hours every night and maintaining a consistent routine of going to bed, waking up.
- Staying active both physically and socially: Getting out of the house every day, going to work, and engaging in social interaction.
Therefore, the Monsenso solution includes five core features that support a patient’s self-management:
- Self-assessments – Reminded by an alarm, patients enter subjective data directly into the system through their smartphones. This data includes mood, sleep, level of activity, and medication. Some items can be customized to accommodate a patient’s specific needs, while others are consistent to provide statistical analysis.
- Activity monitoring – Through a GPS and accelerometer, objective data is collected to monitor a patient’s level of engagement in daily activities. The system can also measure the amount of social activity based on phone calls and text messages.
- Historical overview of data – On the web portal, patients and clinicians can obtain a two-week snapshot of a patient’s basic data for immediate feedback. The portal also gives them access to a detailed historical overview of the data, enabling them to explore it in depth by going back in time, and focusing on specific variables.
- Coaching and self-treatment – The MONARCA systems supported psychotherapy in two ways. Firstly, through customizable triggers that notify the patient and clinician when the data potentially indicates a warning sign. Second, since the patients have access to their own Early Warning Signs, it empowers them to learn more about them.
- Data sharing – To strengthen the relationship between patients and clinicians, important information and treatment decisions are shared.
Resources:
[1] What is bipolar disorder? National Institute of Mental Health. http://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
[2] Bipolar disorder. National Health Service (NHS) UK. http://www.nhs.uk/Conditions/Bipolar-disorder/Pages/Introduction.aspx
[3] Bipolar disorder treatment. HelpGuide.org http://www.helpguide.org/articles/bipolar-disorder/bipolar-disorder-treatment.htm