MHealth, a scalable and cost-efficient solution for mental healthcare
Approximately 450 million people worldwide suffer from mental disorders. One fifth of teenagers under the age of 18 suffer from developmental, emotional or behavioural problems, and one in eight have a mental disorder. Five of the ten leading causes of disability worldwide are psychiatric conditions, including depression, alcohol abuse, schizophrenia, and obsessive compulsive disorder. [1]
The Institute of Medicine Report has proposed a framework of mental health intervention for mental illness based on the classification and the public health distinctions between primary, secondary and tertiary prevention. [1]
Primary prevention focuses on promoting mental well-being, and decreasing adverse conditions such as child abuse, violence, discrimination, poverty, and lack of education to the general population. It also seeks to target individuals or subgroups of the population whose risk of developing a mental illness is higher due to biological, psychological or social risk factors.
Secondary prevention seeks to reduce the symptoms and decrease the number of episodes through early detection and treatment. [1]
Tertiary prevention includes interventions that reduce disability, enhance rehabilitation, and prevent relapses and recurrences of the illness. [1]
A Dutch study found a 50% reduction in the incidence of major depression among mildly depressed primary care patients who received a stepped-care intervention, compared with the incidence among primary care patients who received treatment as usual. Other studies showed that low-dose antidepressants or problem-solving therapy helped reduce the incidence of major and minor depression in post-stroke patients. [2]
Preventive measures such as mental health promotion and early intervention are the most cost-effective way to tackle mental illness on a global scale. Research reveals that common mental disorders such as depression and anxiety can be prevented. For instance, Cognitive Behavioural Therapy (CBT) has proven to be useful for people who already have mild depressive symptoms.
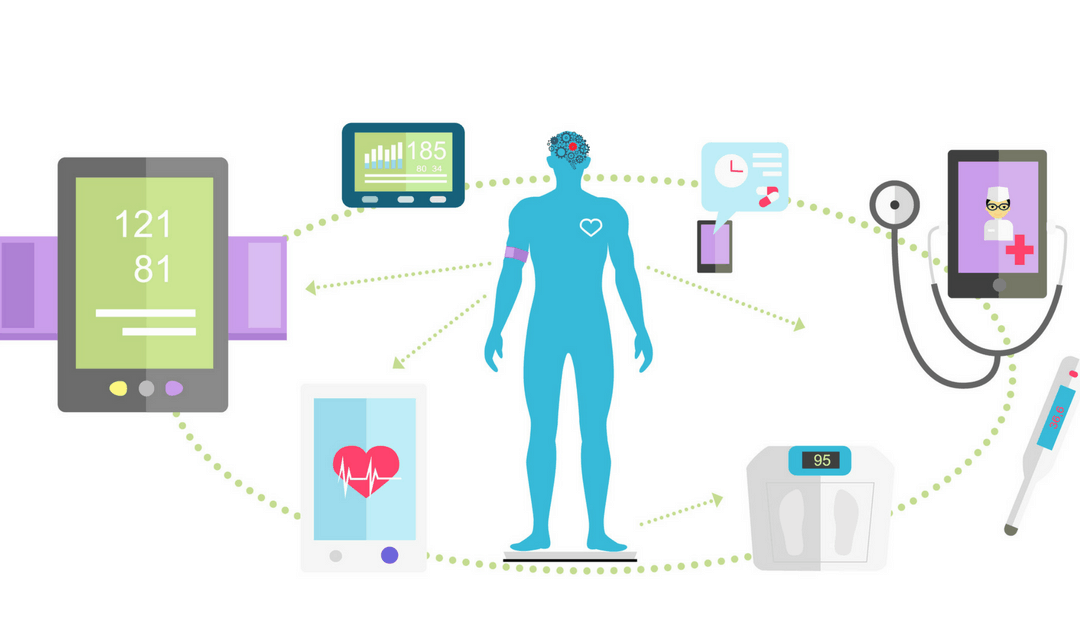
During the last few years, technology has crossed a new frontier in mental health support and data collection. Mobile health (mHealth technology) provides doctors, researchers and the general population with new ways to monitor a patient’s progress, access self-help tools, and increase understanding of mental wellbeing.
Mobile mental health support can be very simple but effective. For example, the Monsenso mHealth solution which consists of a smartphone app for patients and carers and web portal for clinicians uses self-reported data and the device’s built-in sensors to collect patient information. Based on the self-reported data, the Monsenso smartphone app identifies any triggers or warning signs, and it notifies patients and clinicians that help is needed before a crisis occurs. The Monsenso smartphone app also provides users with self-help tools that are always available in case of an emergency.
Although there are many mental health apps available on both the iTunes and Android app stores, this new technology includes a lot of uncertainty. There isn’t enough information on the quality, security and effectiveness of the different apps available, which can confuse clinicians and users.
The advantages of mental health apps
Experts believe that technology has a lot of potential for users and clinicians. A few of the benefits of mobile care include:
- Convenience:Treatment can take place anytime and anywhere (e.g. at home in the middle of the night or on a bus on the way to work) and may be ideal for those who have trouble with in-person appointments.
- Anonymity:Clients can seek treatment options without involving other people.
- An introduction to care: Technology may be a good first step for those who have avoided mental health care in the past.
- Lower cost: Some apps are free or cost less than traditional care.
- Service to more people: Technology can help mental health providers offer treatment to people in remote areas or to many people in times of sudden need (for example following a natural disaster or terror attack).
- Interest: Some technologies might be more appealing than traditional treatment methods, which may encourage clients to continue therapy.
- 24-hour monitoring: Technology can provide round-the-clock monitoring and self-help tools or interventions.
- Consistency: Technology can offer the same treatment plan to all users.
- Support: Technology can complement traditional therapy by extending an in-person session, reinforcing new skills, and providing support and monitoring. [3]
Trends in smartphone apps for mental health
- Self-management apps
Users enter self-reported data into the app so it can provide feedback. For example, medication reminders, stress-coping strategies or sleep problems. Some apps can also track sensor data and may help users monitor their progress and receive feedback. - Apps to improve thinking skills and skills training
Apps that help users with improved thinking skills (cognitive remediation) and learn new coping or thinking skills. For example, they provide educational videos about anxiety management or the importance of social support. Additionally, users might pick up some new skills and use the app to practice those skills. This type of app may feel a little bit like a game, and often target people with severe mental illness. - Supported care
This type of app allows users to interact with a trained health care provider or a peer support group who can offer guidance in case of an emergency. - Monitoring and data collection
This type of mental health app can collect two types of data. On one hand, it gathers data using the sensors built into smartphones such as movement patterns, social interactions, behaviour at different times of the day, speech patterns and more. On the other hand, it collects self-reported data in the form of a mood diary or electronic questionnaire.
Although mental health apps may not replace mental health professionals, they allow clinicians to provide better support to more people regardless of their geographical location.
References:
[1] Prevention of mental disorders. Effective interventions and policy options. World Health Organisation. http://www.who.int/mental_health/evidence/en/prevention_of_mental_disorders_sr.pdf
[2] The future looks promising for mental health prevention. Psychiatric News. Joan Arehart-Treichel. 2013 (January 18). http://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2013.10b1
[3] Technology and the future of mental health treatment. National Institute of Mental Health. http://www.nimh.nih.gov/health/topics/technology-and-the-future-of-mental-health-treatment/index.shtml
